Kp 1.1.3.4 Dan 1.1.3.6 Ebm Pico 5dt6g
This document was ed by and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this report form. Report 3i3n4
Overview 26281t
& View Kp 1.1.3.4 Dan 1.1.3.6 Ebm Pico as PDF for free.
More details 6y5l6z
- Words: 1,443
- Pages: 40
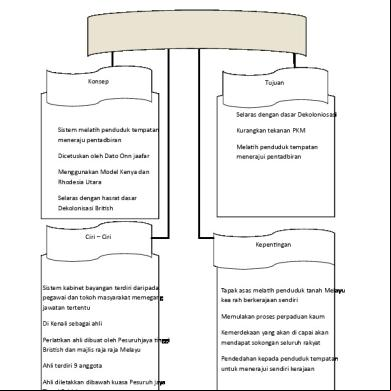
EBM CYCLE AND PICO QUESTION
NAJIRMAN KETUA BAGIAN ILMU PENYAKIT DALAM FK UNAND/ RSUP Dr.M.DJAMIL KEPALA CE-EBM FK UNAND
What is Evidence-based Medicine? Integration of
(1) physician’s competence (2) valid evidence from studies (3) patient’s preference
PEMANFAATAN BUKTI MUTAKHIR YANG SAHIH DALAM TATALAKSANA PASIEN
Evidence-based medicine (EBM) The process of systematically reviewing,
appraising and using clinical research findings to aid the delivery of optimum clinical care to
patients
What is evidence-based medicine? The term ‘evidence-based medicine’ (EBM) was fi rst used by a Canadian, David Sackett and his collegues at McMaster University in Ontario, Canada in the early 1990s EBM as integrating the best research evidence with clinical expertise and patient values to achieve the best possible patient management EBM practitioners to avoid ‘information overload’ but, at the same time, to find and apply the most useful information.
WHY DO WE NEED EBM? There is a large information gap between research and clinical practice
So much research is published all the time, clinicians understandably are unaware of most of it, or do not have the ‘tools’ to assess its quality Researchers, on the other hand, do not understand the information needs of clinicians and continue to present their work in a way that is not easily accessible to busy practitioners Most treatment-related decisions were based on an ad hoc selection of information from the vast and variable quality scientific literature, on expert opinion, or, worse of all, on trial and error
WHY EBM? 1. Information overload 2. Keeping current with literature 3. Our clinical performance deteriorates with time (“the slippery slope”) 4. Traditional CME does not improve clinical performance 5. EBM encourages self directed learning process which should overcome the above shortages
5000/ DAY 5000 4500 4000 3500 3000
2500 2000 1500
1000/ DAY
1000 500
50/DAY
0 TRIALS
MEDLINE
TOTAL
THE AMOUNT OF MEDICAL RESEARCH
Archie Cochrane proposed that researchers and practitioners should collaborate internationally to systematically review all the best clinical trials (that is, randomised controlled trials, or RCTs), specialty by specialty
STEPS IN EBM 1. Formulate an answerable question 2. Track down the best evidence of outcomes available.
3. Critically appraise the evidence (ie find out how good it is). 4. Apply the evidence (integrate the results with clinical expertise and patient values). 5. Evaluate the effectiveness and efficiency of the process (to improve next time).
Drawing conclusion That impact on practice
APPRISING THE EVIDENCE
•Hierarchy of evidence •Pre appraised resources
PATIENT ENCOUNTER
EBM
SEARCHING THE EVIDENCE
Diagnosis Therapy Prognosis Etiology
FORMULATING CLINICAL QUESTIONS
•Patient •Intervention •Comparison •Outcome
CLINICAL EXPERTISE
BEST RESEARCH EVIDENCE
E
PATIENT
B
VALUES &
M
PREFERENCES
STEPS IN EBM PRACTICE 1.
Formulate clinical problems in answerable questions
2.
Search the best evidence: use internet or other online database for current evidence
3.
Critically appraise the evidence for
Validity
(was the study valid?)
Importance
(were the results clinically important?)
Applicability (could we apply to our patient?)
4.
Apply the evidence to patient
5.
Evaluate our performance
LANGKAH PERTAMA
Clinical question = Pertanyaan klinis Disusun menurut rumus : PICO
P = Population/ participants
Who are the relevant patients?
I = Intervention Indicator/
What is the management strategy, diagnostic test or exposure that you are interested in (such as a drug, food, surgical procedure, diagnostic test or exposure to a chemical)?
C = Comparator/ Control
What is the control or alternative management strategy, test or exposure that you will be comparing the one you are interested in with?
O = Outcome
What are the patient-relevant consequences of the exposure in which we are interested?
In EBM, treatments and therapies are called ‘interventions’ and such questions are questions of INTERVENTION Other types of questions that may arise are as follows: 1. What causes the problem? AETIOLOGY AND RISK FACTORS 2. What is the frequency of the problem? FREQUENCY 3. Does this person have the problem? DIAGNOSIS 4. Who will get the problem? PROGNOSIS AND PREDICTION
Interventions Interventions cover a wide range of activities from drug treatments and other clinical therapies, to lifestyle changes (for example, diet or exercise) and social activities (such as an education program). Interventions can include individual patient care or population health activities (for example, screening for diseases such as cervical or prostate cancer).
Example 1 A 28-year-old male presents with recurrent furunculosis for past 8 months; these episodes have been treated with drainage and several courses of antibiotics but keep recurring. He asks if recurrences can be prevented. To convert this to an answerable question, use the P I C O method as follows : P I C O
Population/patient = patients with recurrent furunculosis Intervention/indicator = prophylactic antibiotics Comparator/control = no treatment Outcome = reduction in recurrence rate of furunculosis
Question: ‘In patients with recurrent furunculosis, do prophylactic antibiotics, compared to no treatment, reduce the recurrence rate?’
P = Population, patients, partricipants, problem •Wanita dengan osteoartritis I = Intervention, indicator, index •Temberian steorid C = Comparison •Tanpa steroid
PERTANYAAN KLINIS Pada wanita dengan osteoartritis, O = Outcome apakah pemberian steroid, •Mengurangi nyeri dibanding tanpa steroid, dapat mengurangi keluhan nyeri?
P = Population, patients, partricipants, problem •Pasien dengan tumor tiroid I = Intervention, indicator, index •pemeriksaan USG C = Comparison •biopsi tiroid O = Outcome •menentukan keganasan
PERTANYAAN KLINIS Pada pasien dengan tumor tiroid, apakah pemeriksaan USG lebih sensitif, dibanding dengan biopsi, untuk menegakkan diagnosis keganasan?
P = Population, patients, partricipants, problem •Manula dengan batuk kronik berulang I = Intervention, indicator, index •fisioterapi
PERTANYAAN KLINIS Pada manula dengan C = Comparison batuk berulang, apakah •tanpa fisio terapi fisioterapi dapat O = Outcome empercepat •mempercepat kesembuhan kesembuhan?
P = Population, patients, partricipants, problem •Pasien lupus eritematosus sistemik I = Intervention, indicator, index •riwayat gagal jantung C = Comparison •tanpa riwayat gagal jantung O = Outcome •memperburuk prognosis
PERTANYAAN KLINIS Pada pasien LES apakah terdapatnya riwayat gagal jantung memperburuk prognosis?
AETIOLOGY AND RISK FACTORS Example 1 George has come in to your surgery to discuss the possibility of getting a vasectomy. He says he has heard something about vasectomy causing an increase in testicular cancer later in life.
You know that the risk of this is low but want to give him a more precise answer.
P Population/patient = adult males I Intervention/indicator = vasectomy C Comparator/control = no vasectomy OOutcome = testicular cancer
Question: ‘In men, does having a vasectomy (compared to not having one) increase the risk of getting testicular cancer in the future?’
FREQUENCY OR RATE Questions of frequency (prevalence) are about how many
people in the population have a disease or health problem, such as what is the frequency of hearing problems in infants or the prevalence of Alzheimer’s disease in the over 70s. If the question also includes a time period, such as for cases of influenza in winter versus summer, it becomes a question of rate (incidence).
Example 1 Mabel is a 6-week-old baby at her routine follow-up. She was born prematurely at 35 weeks. You want to tell the parents about her chances of developing hearing problems. P = infants I = premature C = full-term
Question: ‘In infants born prematurely, compared to those born at full term, what will the prevalence of sensorial deafness be?’
O = sensorial deafness
APLIKASI EBM DALAM PELAYANAN KESEHATAN
Evidence
Physician
Patients
EBM
Type of Clinical Questions for the Ideal Type of Study
Type of Question Ideal Type of Study
Therapy
RCT > Cohort Study > Case Control
Diagnosis:
Prospective, blind controlled trial comparison to gold standard
Prognosis
Cohort Study > Case Control > Case Series/Case Report
Etiology/Harm
RCT > Cohort Study > Case Control
Levels of Evidence: Study Type / Evidence Hierarchy
JENIS DISAIN PENELITIAN CROSS SECTIONAL/ POTONG LINTANG CASE CONTROL COHORT
CLINICAL TRIAL/ EXPERIMENTAL
Level bukti (level of evidence) untuk efek terapi Level Desain/ jenis studi Level I RCT berkualitas tinggi dengan perbedaan yang secara statistik signifikan, atau perbedaan yang secara statistik tidak signifikan tetapi dengan Confidence Interval sempit Kajian sistematis dari RCT level I (dan hasil studi homogen) Level II RCT dengan kualitas lebih rendah (misalnya, follow-up <80%, tanpa pembutaan, atau randomisasi tidak sempurna) Studi prospektif dengan pembanding Kajian sistematis dari studi level II atau studi level I dengan hasil-hasil inkonsisten Level III Studi kasus kontrol Studi retrospektif dengan pembanding Kajian sistematis dari studi level III Level IV Case series Level V Pendapat pakar Sumber: deVries dan Berlet, 2010
SEARCHING
Kapankah perlu dibuat pertanyaan klinis ? Pertanyaan klinis perlu dibuat bila: • penting untuk kesembuhan pasien • diperkirakan akan ditemukan jawabannya • sering dijumpai dalam praktik • menarik untuk kita • ada kemungkinan berkaitan dengan isu medikolegal PANDUAN PRAKTEK KLINIK
LOGO
NAJIRMAN KETUA BAGIAN ILMU PENYAKIT DALAM FK UNAND/ RSUP Dr.M.DJAMIL KEPALA CE-EBM FK UNAND
What is Evidence-based Medicine? Integration of
(1) physician’s competence (2) valid evidence from studies (3) patient’s preference
PEMANFAATAN BUKTI MUTAKHIR YANG SAHIH DALAM TATALAKSANA PASIEN
Evidence-based medicine (EBM) The process of systematically reviewing,
appraising and using clinical research findings to aid the delivery of optimum clinical care to
patients
What is evidence-based medicine? The term ‘evidence-based medicine’ (EBM) was fi rst used by a Canadian, David Sackett and his collegues at McMaster University in Ontario, Canada in the early 1990s EBM as integrating the best research evidence with clinical expertise and patient values to achieve the best possible patient management EBM practitioners to avoid ‘information overload’ but, at the same time, to find and apply the most useful information.
WHY DO WE NEED EBM? There is a large information gap between research and clinical practice
So much research is published all the time, clinicians understandably are unaware of most of it, or do not have the ‘tools’ to assess its quality Researchers, on the other hand, do not understand the information needs of clinicians and continue to present their work in a way that is not easily accessible to busy practitioners Most treatment-related decisions were based on an ad hoc selection of information from the vast and variable quality scientific literature, on expert opinion, or, worse of all, on trial and error
WHY EBM? 1. Information overload 2. Keeping current with literature 3. Our clinical performance deteriorates with time (“the slippery slope”) 4. Traditional CME does not improve clinical performance 5. EBM encourages self directed learning process which should overcome the above shortages
5000/ DAY 5000 4500 4000 3500 3000
2500 2000 1500
1000/ DAY
1000 500
50/DAY
0 TRIALS
MEDLINE
TOTAL
THE AMOUNT OF MEDICAL RESEARCH
Archie Cochrane proposed that researchers and practitioners should collaborate internationally to systematically review all the best clinical trials (that is, randomised controlled trials, or RCTs), specialty by specialty
STEPS IN EBM 1. Formulate an answerable question 2. Track down the best evidence of outcomes available.
3. Critically appraise the evidence (ie find out how good it is). 4. Apply the evidence (integrate the results with clinical expertise and patient values). 5. Evaluate the effectiveness and efficiency of the process (to improve next time).
Drawing conclusion That impact on practice
APPRISING THE EVIDENCE
•Hierarchy of evidence •Pre appraised resources
PATIENT ENCOUNTER
EBM
SEARCHING THE EVIDENCE
Diagnosis Therapy Prognosis Etiology
FORMULATING CLINICAL QUESTIONS
•Patient •Intervention •Comparison •Outcome
CLINICAL EXPERTISE
BEST RESEARCH EVIDENCE
E
PATIENT
B
VALUES &
M
PREFERENCES
STEPS IN EBM PRACTICE 1.
Formulate clinical problems in answerable questions
2.
Search the best evidence: use internet or other online database for current evidence
3.
Critically appraise the evidence for
Validity
(was the study valid?)
Importance
(were the results clinically important?)
Applicability (could we apply to our patient?)
4.
Apply the evidence to patient
5.
Evaluate our performance
LANGKAH PERTAMA
Clinical question = Pertanyaan klinis Disusun menurut rumus : PICO
P = Population/ participants
Who are the relevant patients?
I = Intervention Indicator/
What is the management strategy, diagnostic test or exposure that you are interested in (such as a drug, food, surgical procedure, diagnostic test or exposure to a chemical)?
C = Comparator/ Control
What is the control or alternative management strategy, test or exposure that you will be comparing the one you are interested in with?
O = Outcome
What are the patient-relevant consequences of the exposure in which we are interested?
In EBM, treatments and therapies are called ‘interventions’ and such questions are questions of INTERVENTION Other types of questions that may arise are as follows: 1. What causes the problem? AETIOLOGY AND RISK FACTORS 2. What is the frequency of the problem? FREQUENCY 3. Does this person have the problem? DIAGNOSIS 4. Who will get the problem? PROGNOSIS AND PREDICTION
Interventions Interventions cover a wide range of activities from drug treatments and other clinical therapies, to lifestyle changes (for example, diet or exercise) and social activities (such as an education program). Interventions can include individual patient care or population health activities (for example, screening for diseases such as cervical or prostate cancer).
Example 1 A 28-year-old male presents with recurrent furunculosis for past 8 months; these episodes have been treated with drainage and several courses of antibiotics but keep recurring. He asks if recurrences can be prevented. To convert this to an answerable question, use the P I C O method as follows : P I C O
Population/patient = patients with recurrent furunculosis Intervention/indicator = prophylactic antibiotics Comparator/control = no treatment Outcome = reduction in recurrence rate of furunculosis
Question: ‘In patients with recurrent furunculosis, do prophylactic antibiotics, compared to no treatment, reduce the recurrence rate?’
P = Population, patients, partricipants, problem •Wanita dengan osteoartritis I = Intervention, indicator, index •Temberian steorid C = Comparison •Tanpa steroid
PERTANYAAN KLINIS Pada wanita dengan osteoartritis, O = Outcome apakah pemberian steroid, •Mengurangi nyeri dibanding tanpa steroid, dapat mengurangi keluhan nyeri?
P = Population, patients, partricipants, problem •Pasien dengan tumor tiroid I = Intervention, indicator, index •pemeriksaan USG C = Comparison •biopsi tiroid O = Outcome •menentukan keganasan
PERTANYAAN KLINIS Pada pasien dengan tumor tiroid, apakah pemeriksaan USG lebih sensitif, dibanding dengan biopsi, untuk menegakkan diagnosis keganasan?
P = Population, patients, partricipants, problem •Manula dengan batuk kronik berulang I = Intervention, indicator, index •fisioterapi
PERTANYAAN KLINIS Pada manula dengan C = Comparison batuk berulang, apakah •tanpa fisio terapi fisioterapi dapat O = Outcome empercepat •mempercepat kesembuhan kesembuhan?
P = Population, patients, partricipants, problem •Pasien lupus eritematosus sistemik I = Intervention, indicator, index •riwayat gagal jantung C = Comparison •tanpa riwayat gagal jantung O = Outcome •memperburuk prognosis
PERTANYAAN KLINIS Pada pasien LES apakah terdapatnya riwayat gagal jantung memperburuk prognosis?
AETIOLOGY AND RISK FACTORS Example 1 George has come in to your surgery to discuss the possibility of getting a vasectomy. He says he has heard something about vasectomy causing an increase in testicular cancer later in life.
You know that the risk of this is low but want to give him a more precise answer.
P Population/patient = adult males I Intervention/indicator = vasectomy C Comparator/control = no vasectomy OOutcome = testicular cancer
Question: ‘In men, does having a vasectomy (compared to not having one) increase the risk of getting testicular cancer in the future?’
FREQUENCY OR RATE Questions of frequency (prevalence) are about how many
people in the population have a disease or health problem, such as what is the frequency of hearing problems in infants or the prevalence of Alzheimer’s disease in the over 70s. If the question also includes a time period, such as for cases of influenza in winter versus summer, it becomes a question of rate (incidence).
Example 1 Mabel is a 6-week-old baby at her routine follow-up. She was born prematurely at 35 weeks. You want to tell the parents about her chances of developing hearing problems. P = infants I = premature C = full-term
Question: ‘In infants born prematurely, compared to those born at full term, what will the prevalence of sensorial deafness be?’
O = sensorial deafness
APLIKASI EBM DALAM PELAYANAN KESEHATAN
Evidence
Physician
Patients
EBM
Type of Clinical Questions for the Ideal Type of Study
Type of Question Ideal Type of Study
Therapy
RCT > Cohort Study > Case Control
Diagnosis:
Prospective, blind controlled trial comparison to gold standard
Prognosis
Cohort Study > Case Control > Case Series/Case Report
Etiology/Harm
RCT > Cohort Study > Case Control
Levels of Evidence: Study Type / Evidence Hierarchy
JENIS DISAIN PENELITIAN CROSS SECTIONAL/ POTONG LINTANG CASE CONTROL COHORT
CLINICAL TRIAL/ EXPERIMENTAL
Level bukti (level of evidence) untuk efek terapi Level Desain/ jenis studi Level I RCT berkualitas tinggi dengan perbedaan yang secara statistik signifikan, atau perbedaan yang secara statistik tidak signifikan tetapi dengan Confidence Interval sempit Kajian sistematis dari RCT level I (dan hasil studi homogen) Level II RCT dengan kualitas lebih rendah (misalnya, follow-up <80%, tanpa pembutaan, atau randomisasi tidak sempurna) Studi prospektif dengan pembanding Kajian sistematis dari studi level II atau studi level I dengan hasil-hasil inkonsisten Level III Studi kasus kontrol Studi retrospektif dengan pembanding Kajian sistematis dari studi level III Level IV Case series Level V Pendapat pakar Sumber: deVries dan Berlet, 2010
SEARCHING
Kapankah perlu dibuat pertanyaan klinis ? Pertanyaan klinis perlu dibuat bila: • penting untuk kesembuhan pasien • diperkirakan akan ditemukan jawabannya • sering dijumpai dalam praktik • menarik untuk kita • ada kemungkinan berkaitan dengan isu medikolegal PANDUAN PRAKTEK KLINIK
LOGO