Nursing Responsibilities During Radiation Therapy 6j2m3n
This document was ed by and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this report form. Report 3i3n4
Overview 26281t
& View Nursing Responsibilities During Radiation Therapy as PDF for free.
More details 6y5l6z
- Words: 14,588
- Pages: 59
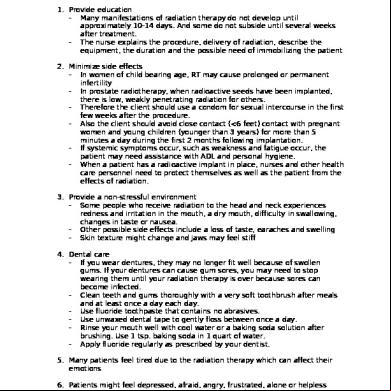
NURSING RESPONSIBILITIES DURING RADIATION THERAPY 1. Provide education - Many manifestations of radiation therapy do not develop until approximately 10-14 days. And some do not subside until several weeks after treatment. - The nurse explains the procedure, delivery of radiation, describe the equipment, the duration and the possible need of immobilizing the patient 2. Minimize side effects - In women of child bearing age, RT may cause prolonged or permanent infertility - In prostate radiotherapy, when radioactive seeds have been implanted, there is low, weakly penetrating radiation for others. - Therefore the client should use a condom for sexual intercourse in the first few weeks after the procedure. - Also the client should avoid close (<6 feet) with pregnant women and young children (younger than 3 years) for more than 5 minutes a day during the first 2 months following implantation. - If systemic symptoms occur, such as weakness and fatigue occur, the patient may need assistance with ADL and personal hygiene. - When a patient has a radioactive implant in place, nurses and other health care personnel need to protect themselves as well as the patient from the effects of radiation. 3. Provide a non-stressful environment - Some people who receive radiation to the head and neck experiences redness and irritation in the mouth, a dry mouth, difficulty in swallowing, changes in taste or nausea. - Other possible side effects include a loss of taste, earaches and swelling - Skin texture might change and jaws may feel stiff 4. Dental care - If you wear dentures, they may no longer fit well because of swollen gums. If your dentures can cause gum sores, you may need to stop wearing them until your radiation therapy is over because sores can become infected. - Clean teeth and gums thoroughly with a very soft toothbrush after meals and at least once a day each day. - Use fluoride toothpaste that contains no abrasives. - Use unwaxed dental tape to gently floss between once a day. - Rinse your mouth well with cool water or a baking soda solution after brushing. Use 1 tsp. baking soda in 1 quart of water. - Apply fluoride regularly as prescribed by your dentist. 5. Many patients feel tired due to the radiation therapy which can affect their emotions 6. Patients might feel depressed, afraid, angry, frustrated, alone or helpless - Peer groups may meet at your hospital
-
Emotional and spiritual encouragement also is important to the healing process.
7. Side effects can include eating and digestion problems. You may completely lose interest in food during your treatment. - Even if you are not hungry, it is important to keep your protein and calorie intake high. - Doctors have found that patients who eat can better handle their cancers and side effects. - Eat when you are hungry, even when it is not meal time. - Eat several small meals during the day rather than 2 or 3 large meals. - Vary your diet and try new recipes. - If you don’t drink alcohol, ask your doctor if you should avoid alcohol during your treatment. - Keep healthful snacks close by nibbling when you get the urge. Drink milkshakes or prepared liquid supplements between meals. Patient receives a low residue diet to prevent frequent bowel movements. Radiation therapy may cause anorexia which may lead to inadequate nutrition and hydration so small frequent feedings or use of nutritional supplements may be required to maintain adequate nutrition. In radiation therapy, fatigue or malaise also contribute to poor nutritional intake thus planned rest periods may provide relief of fatigue providing increased energy for meal preparation or consumption. Nutrition – to promote retention of nutrients, ister antiemetics as prescribed. Encourage high calorie meals when child is least likely to be nauseated. Praise a child’s effort to eat. Provide foods identified by child as special favorites. Serve easy to swallow food at tolerable temperature. If mucous membrane of mouth, pharynx or esophagus is irradiated, modification of diet to bland, soft, or liquid foods will be necessary; mouth is rinsed frequently with a mild alkaline mouthwash; teeth are gently cleansed with absorbent cotton or gauze rather than the usual brush. Avoids foods that are dry and thick. 8. For lactating mothers undergoing radiation therapy. - Advise pt. not to breastfeed to prevent adverse effects to fetus. - Advise pt. to drink plenty of fluids to prevent dehydration. - Monitor nutritional status. 9. Miscellaneous. - A urinary catheter will be in place (if ordered) and must be inspected frequently to ensure that it drains properly. - Any profuse discharge should be reported immediately to the radiation oncologist or gynecologic surgeon.
-
-
-
-
Observing the patient for temperature elevation, nausea, and vomiting. The symptoms may indicate such complications as infection. Patient teaching includes informing the patient that abdominal fullness, cramping, backache, and the urge to void are normal feelings during therapy. Severe should not occur. Mild opioid agents, muscle relaxants or sedative medications may be helpful. Private room, with private bathroom and facilities Room previously occupied with patients previously treated with radionuclide treatment should not be used until the room has been cleansed and surveyed for residual contamination. Items such as bedpans, urinals and basins if disposable may be disposed of as radioactive waste. If these items are not disposable, they shall be thoroughly washed with soap and running water. Any vomitus, gastric contents collected during the first 24 hours by nasogastric aspiration or excessive sputum should be collected in a waterproof container and held for disposal by radiation safety division personnel. Wearing of lead apron The nurse must deal safety with radioactive body discharges by wearing gloves and in some instances placing excreta in containers for special disposal. For a child receiving radiation therapy Provide ample time to answer questions of children undergoing radiation therapy Advise client to wear loose clothing as skin in the area being treated might become more sensitive to touch. Skin changes: The patient is observed for possible reactions: Slight redness for a brief period Transitory epilation Erythema with temporary sweat gland activity suppression Dry desquamation For large doses or sensitive skin; observe the following: Marked erythema followed by purple discoloration Blister formation and moist desquamation Slow healing, leaving skin atrophied, thin and very sensitive to heat, cold and trauma. Permanent epilation and sweat gland destruction After treatment, the area is gently cleansed with tepid water and patted dry; soap is not used and brisk rubbing is avoided. Alcohol, powders, oils, lotions, creams, ointments, deodorants are not used unless prescribed by the doctor. The site is kept dry and may be covered lightly with smooth cloth/cotton but adhesive tape is contraindicated, used an alternative instead. If larynx is treated with radiation, the patient is closely observed 3-4 days for any difficulty in breathing; edema may develop and occlude airway necessitating prompt intubation or a tracheostomy.
-
Frequent blood cell counts are done because the hemapoetic tissue is extremely sensitive to radiation. with persons with an infection should be avoided especially with respiratory infection because of the patients lowered resistance. Patient should have an extra rest, increased fluid intake and a high calorie, high protein, high vitamin diet. If the patient is allowed to go home, the importance of keeping the appointments for his treatments is stressed. Internal Radiation Therapy: - Patient should receive a simple explanation of the procedure and necessary precautions so he will know what to expect and what is expected of him. - Time is taken to answer his questions and dispel misconceptions. - After implantation, temperature is taken every 4 hours, an increase over 38 degrees is perorted. - Any radioactive material should be handled with a long forceps, never with hands. - All dressings should be checked before disposal. - Patient’s visitors are required to maintain a 3 feet distance from the patient. - Health workers should know the time at which the radioactive implant is to be removed and should have necessary equipment in advance and to remind the person responsible for removal. Nursing responsibilities for the patient receiving radiation therapy
Teletherapy The radiation source is exterior to the tumor such as the use of linear accelerator. 1. Remove all opaque objects such as pins, buttons and hairpins and replace clothing with a gown for body X-rays. 2. Have patient perfectly still; maintain position with the use of foam, plastic, plaster (material) devices and/or variety of other materials that can conform to the patient’s anatomy. 3. Tell the patient there will be no sensation or pain accompanying radiation therapy. 4. Advise the patient that he will be alone in the room for the protection of the technician, but will be in voice . 5. Determine from the physician what has been told to the patient about radiation therapy 6. If series of treatments are to be given, include the patient in the planning phase. Brachytherapy - The radiation source is used for surface, interstitial, or intracavity applications 1. The nurse should inform the patient that some skin reaction can be expected but that varies from patient to patient. 2. Do not apply lotions, ointments, cosmetics, etc. to the site of radiation unless prescribed by the physician. Cornstarch may be used when the skin
is dry and or itchy. Discourage vigorous rubbing or scratching. It may destroy skin cells. Techniques while working with patients undergoing radiation therapy: 1. Put on shoe covers and protective gloves before entering patients room. 2. Work quickly but effectively and courteously. Minimize your time in the room. 3. Note: No matter how long you are in the room, you will not receive a radiation exposure large enough to cause adverse effects. 4. Leave all trash, linens, and food trays in the room 5. After leaving the room, wash your hands. 6. Personnel should not smoke, eat or drink in areas where unencapsulated radio active is used in patient treatment or if the possibilities of contamination of the hands persist. General procedures for obtaining specimens from therapy patients 1. Read the instructions posted in the door. 2. Specimen containers must be labeled with radioactive material labels or tape to identify them as radioactive. 3. Put on a face mask if the patient has a tracheostomy or has symptoms of a respiratory infection. 4. Never use sink for handwashing/ use telephone/ cellphones while in the room. Nursing considerations in external radiotherapy: 1. It is important that the patient receive an explanation of the procedure and precautions. 2. Orient the patient and his family in advance, answer their questions and reassure them that the treatments are well controlled and adequate protection is used. 3. Following the treatment, observe for possible reactions. 4. Instruct and suggest care of the skin 5. Avoid patient to with other persons with infections 6. General ive care applicable to all patients receiving radiotherapy include extra rest, an increase fluid intake and a high calorie, high protein, high vitamin diet 7. When reaction develops, reassure that they are not unexpected and are not an indication of a recurrence or worsening of his cancerous disease. Nursing responsibilities in internal radiotherapy: 1. An explanation to the patient of the procedure and the precautions 2. Place the patient in isolation in a single room and indicate that no visitors are allowed 3. Provide a telephone and radio or television and reading materials 4. In close with patient always wear a lead apron or gown and rubber gloves 5. Wear a monitoring badge which records the amount of radiation received by the patient 6. Visit patient once in a while 7. Nurse should wash hands thoroughly after any with patient and other equipment
8. Linens, dishes, syringes, needles and other treatment equipment are monitored before being returned. For infants and children - No cream, no lotion should be applied to radiation areas until the treatment series is completed. - If creams contain any metal, these could distort or interfere with the entrance of radiation. - If the head will be irradiated, a dental consult may be suggested. This can slow healing of a tooth extraction. During treatment: - Require them to be still for a period of time possibly on an uncomfortable table. - Assure patients and the child that during the treatment, just as there is no sensation from x-ray exposure, the child may will experience no sensation from radiation exposure. - Infants are usually prescribed a sedative or conscious sedation before therapy to ensure that they be still during the procedure. - To make this approach affective, keep the child fairly active early in the day and introduce activities after the sedative is istered. After treatment: - If head is involved in therapy, alopecia (hair loss) may result. - Radiation to the head may reduce salivary gland function, leading to a constantly dry mouth. - Tooth growth may be halted due to root therapy. - Radiation to bone marrow may depress blood cell and platelet production. - Children undergoing radiation therapy need their leukocytes and platelet counts monitored periodically for changes. For clients undergoing radiation: - Clients with radioactive implants are a source of radiation to the immediate environment. - The nurse who is in close with such clients also needs to wear a lead apron. - Nurses must deal safely with radioactive body discharges by wearing gloves and in some instances placing excreta in containers for special disposal. - The nurse must wash gloved hands well before and after removing the gloves and placed contaminated materials in a special containers for special disposal. - Nurses must make sure they understand treatment and the precautions they need to take. Often such clients are restricted to bed or to a confined area to protect others. - These clients need emotional to deal with the precautions and will likely accept treatments and precautions better when they know what will happen, when and why. - Exposure of the reproductive organs of mice and rabbits to X rays has caused gene mutations that resulted in malformed offsprings and geneticist believe that comfortable effects can occur in humans.
-
Knowing these, great care is taken to protect both the nurse and patient from unnecessary exposure.
-
Chemotherapy and radiation therapy: knowledge of the appropriate routes, doses and reactions is required. Infection control: nurses must be aware of standard infection control precautions. Nausea and vomiting are most likely to occur when the radiation dose is high or if the abdomen or another part of the digestive tract is irradiated. Sometimes nausea and vomiting occur after radiation to other regions, but in these cases the symptoms usually disappear within a few hours after treatment. Nausea and vomiting can be treated with antacids, Compazine, Tigan or Zafran. Fatigue frequently starts after the 2nd week therapy and may continue until about 2 weeks after the therapy is finished. Patients may need help to limit their activities, take naps and get extra sleep at night.
-
-
Nursing Diagnoses and its Nursing Interventions
-
Nursing Diagnosis: Impairment of skin integrity due to irradiation Nurisng interevntions: - For patients with xerostomia undergoing irradiation - Patient education - Nursing care involves assesing the physical and emotional aspects of the patient before, during and after a course of head and neck irradiation, and providing interventions, education and . - During radiation therapy, the patient should be very gentle with the skin in the treatment area. This nurses can suggest the following: Avoid irritatitng treated skin. When washing, use only lukewarm water and mild soap, pat dry. Do not wear tight clothing over the area. Do not rub, scrub or scratch the skin in the treatment area. Avoid putting anything that is hot or cold, such as heating pad or ice packs on treagted skin. Ask the doctor or nurse to recommend skin care products that will not cause skin irritation. Do not use any powders, creams, perfumes, deodorants, body oils, ointments, lotions or home remedies in the treatment area while you’re being treated and for several weeks afterward unless approved by the doctor. Do not apply skin lotion within 2 hours of treatment. Avoid exposing the radiated area to the sun during treatment, after is over, ask the doctor or nurses how long you should continue to take extra precautions in the sun. Avoid extremes of temperature Avoid rough and tight garments. Avoid rubbing or scratching the area the nurse needs to explain that during treatment, the patient must stay in absolute bedrest.
-
Nurses should know also that over exposure to radiation may include burning and scarring of the skin or lungs; a tendency to develop cataracts; a tendency to develop cancer; to destroy blood producing tissue.
-
Use only luke warm water and mild soap. Just let water run over the treated area. Do not rub. Do not wear tight clothing over the treatment area. Try not to rub, scrub or scratch any sensitive spots. Avoid exposing the area to the sun during treatment and for at least 1 year after the treatment is completed. If you expect to be in the sun for more than a few minutes, wear protective clothing and sunscreen. Ask your doctor or nurse ing sunscreen lotions. Wash the irritated area gently each day with sitter water alone on a mild soap and water. Use your hand rather than a washcloth to be more gentle. Rinse soap thoroughly from your skin. Take care not to remove the markings that indicate exactly where the beam of radiation is to be focused. Dry the irradiated area with potting motions rather than rubbing motions, using a clean, soft towel Use no powders, ointments, lotions, or creams on your skin at the radiation site unless they are prescribed by your radiologist. Wear soft clothing over the skin at the radiation site. Avoid exposure of the irradiated area to the sun. A void heat exposure. Mild erythema to moist desquamation similar to appearance to a second-degree burn. The nurse assesses the patient’s skin, nutritional status and general feeling of well being. The skin and oral mucosa are assesses frequently for changes. The skin is protected from irritation and the patient is instructed to avoid using ointments, lotion or powder on the area. Pressure is avoided by avoiding tight clothing’s and prolonged lying on the area of treatment. No hot or cold is applied on the site and must be protected from direct sunlight. If itching and irritation accompanying erythema, you may suggest application of plain calamine lotion without phenol; or cornstarch. • Dryness and pruritus may occur at an accumulated dose of 2000 to 28000 Cgy (1.2) and is caused by obliteration of sebaceous glands within the field. • This is an acute phenomenon that correlates with the depletion of actively proliferating basal cells in the epidermal layer of the skin, a fixed percentage of which die with each dose fraction of irradiation. • Remaining basal cells are stimulated and their cell cycle shortened. • Subsequent peeling of the skin is defined as dry desquamation. • The skin becomes dry and patient may notice itching and burning sensations.
-
•
Dry skin is susceptible to further injury through scratching and/or formation of fissures – augmenting the risk of infection and tissue necrosis.
Nursing Diagnosis: Potentials for infection due to bone marrow depression Nursing Intervention: - Monitor blood counts weekly. - Teach person to avoid infection by frequent handwashing and good nutrition, hygiene and good habits. - Teach persons signs of infection to report to physician. Nursing Diagnosis: Potential for bleeding due to BM depression: Nursing Interventions: - Monitor platelet counts weekly - Teach person to avoid physical trauma and aspirin while platelets are low - Teach person signs of hemorrhage to report to physician - Monitor stool, integument for signs of hemorrhage - Use direct pressure over injection sites until bleeding stops Nursing Diagnosis: Activity intolerance due to anemia Nursing intervention: - Discuss fatigue and its causes with person - Encourage good nutrition and plenty of rest Nursing Diagnosis: Alteration in Nutrition: Less than body requirements due to anemia Nursing intervention: - Monitor diet for efficient calories - dietitian if indicated - Monitor weight weekly or daily - Assess person’s understanding of nutrition and teach as necessary Nursing Diagnosis: Alteration in mucous membranes due to irradiation Nursing interventions: - Monitor oral cavity daily - Encourage bland diet, no smoking, no alcohol - Good oral hygiene and saline rinses every 2 hours while awake may help - Ensure professional dental care - Avoid foods that are dry and thick Care of the teeth, gums, mouth and throat - Avoid spices and coarse foods such as raw vegetables, dry crackers and nuts - Do not eat or drink very hot foods - Do not smoke, chew tobacco or drink alcohol because tobacco and alcohol can further irritate mouth sores. - Stay away from sugary foods and snacks. - Ask your doctor or nurse to recommend a good mouthwash. The alcohol content in some mouthwashes has a drying effect on mouth tissues. - Sip cool drinks often throughout the day. - Eat or chew sugar free candy or gum to help keep your mouth moist
- Moisten food with gravies and sauces to make eating easier. - Gentle oral hygiene is essential to remove debris, prevent irritation and promote healing Mucositis: do not remove membrane Nursing Diagnosis: Alteration in bowel elimination: diarrhea due to irradiation Nursing interventions: - Monitor stool - Give low residue diet/antidiarrhea medication as prescribed. Nursing Diagnosis: Alteration in comfort and vomiting due to irradiation Nursing interventions: - Plan rest periods before and after meals - ister antiemetics as prescribed - Monitor fluids and electrolytes Nursing Diagnosis: Alteration in comfort: headache due to irradiation Nursing Interventions: - Monitor pain - ister analgesics as prescribed Nursing Diagnosis: Disturbance in self concept due to alopecia Nursing interventions: - Encourage verbalization of feelings - Suggest use of wigs, scarf’s, hats, etc - Instruct person on hair care Nursing Diagnosis: Alteration in urinary elimination patterns due to irradiation Nursing interventions: - Monitor urine for blood - Monitor for dysuria or urinary frequency - Encourage fluid intake Nursing Diagnosis: Social isolation due to irradiation Nursing Interventions: - Explain and discuss irradiation precaution - Encourage telephone calls - Suggest television, radio or tape player - Stop by door to say “hello”
HYPERSENSITIVITY REACTIONS
• •
Exaggerated or inappropriate response to specific antigen Anaphylaxis, allergies, transfusion reactions, graft rejections
TYPE I – Anaphylactic / Immediate Hypersensitivity Reaction Common antigens: Insect bites, drugs, food, pollen, x-ray contrast medium Signs and Symptoms: Urticaria(hives) caused by foods- eggs, fish , nuts, drugs Atopic allergies – less severe and more common form seen in about 15% of the population. Atopy means inherited hypersensitivity. Common Antigens include: Inhalants – dust, pollens, mold spore, animal dander ants – fibers in wool, fur, nylon, plant oils, osaps, cosmetics, perfumes, hair dyes, nickel in jewelry, clothings, occupational chemicals, changes in temperature and stress Pathophysiology: IgE attach to the surface of mast cells and basophils providing a site for allergens to bond the cells. This causes the cells to releases vasoactive substances including histamine leading to: 1. Constriction of smooth muscles in the bronchi – bronchospasm 2. Increase in vascular permeability – urticaria(hives or tissue edema 3. Increase in mucus secretions – hay fever and asthma Symptoms: wheezing, sneezing, rhinitis with conjunctivitis; urticaria, angioedema, rash: diarrhea; fever, malaise, t pains, hematopoietic suppression, anaphylaxis Sensitizing Dose – initial with allergen that triggers the synthesis of specific antiallergenic IgE antibodies Shocking, Challenging Dose – subsequent with allergen, indi exhibits the symptoms of Type I Nursing Process: Assessment – history taking Diagnostic Test – skin test, radioallergosorbent test, one-week food diary test Nursing Diagnosis: Alerted health maintenance; Knowledge deficit Implementation: 1. Prevent anaphylactic reaction - Epinephrine; Benadryl; aminophylline, tracheal intubation; shock therapy 2. Allergen immunotherapy 3. Control the environment – house dust; animal dander; pollens; fungus 4. Facilitate learning – remind physician of allergy if new medications are prescribed; read all labels of nonprescription drugs before taking the new drug; examine all labels of new prepared foods for presence of allergens; avoid eating unknown foods when travelling; use non allergenic soaps and cosmetics – coat nickel containing jewelry with clean nailpolish; use gloves to handle allergen; report side effects of prescribed medication
TYPE II – Cytotoxic Hypersensitivity
•
•
Caused by antibodies (IgG and IgM) directed against antigens on a person’s red blood cells, lymphocytes or platelets or tissue cells. The reaction of antibodies and antigens usually leads to activation of the complement system. Damage cells by causing lysis as in compatible blood transfusion reactions
Types of Transfusion Reactions: 1. Acute hemolytic Reaction/hemolytic transfusion reaction - Infusion of ABO incompatible with blood, RBCs or components containing 10 ml or more RBC’s antibodies in the recipients plasma attach to the antigens on transfused RBC’S ---RBC destruction. Chills, fever, low back pain, flushing, tachycardia, tachypnea, hypotension, vascular collapse, hemoglobinuria, bleeding, ARF, shock, cardiac arrest, death 2. Febrile, Non Hemolytic ( most common) - Sensitization to donor’s WBC’s, platelets or plasma proteins - Sudden chills and fever, headache, flushing, anxiety, muscle pain 3. Mild Allergic reaction involves sensitivity to foreign plasma proteins - Flushing, itching, urticaria 4. Anaphylactic reaction - Infusion of IgA protein to IgA deficient recipient who has developed IgA antibody - Anxiety, urticaria, wheezing, tightness and pain chest, difficulty swallowing, progressing to cyanosis, shock and possible cardiac arrest 5. Delayed hemolytic reaction - An amnestic immune response that occurs 7-14 days after transfusion. Sensitization to RBC antigen not ABO system - Fever, chills, back pains, jaundice, anemia, hemoglobinuria 6. Graft-versus-Host Disease_Pt. - Immunodeficient person receives lymphocytes begin to reject cells 4-30 days after the transfusion. - Anorexia, nausea, diarrhea, high fever, rash, stomatitis, liver dysfunction Prevention of transfusion Reaction: Accurate laboratory testing; careful blood istration TYPE III – Hypersensitivitis/Immune Complex - Involves antigens, antibodies (IgG and IgM) and the complement system. When certain ratios of antigen to antibody occur, the immune complexes are small enough to escape phagocytosis, but they become trapped in the basement membrane under the endothelium of blood vessels, where they activate complement and cause inflammation - Glomerulonephritis and rheumatoid arthritis - Antihistamines and salicylates; steroids – prednisone; epinephrine TYPE IV – Cell mediated or Delayed Hypersensitivity Reaction - Usually appears 12-72 hours after exposure to an allergen. Occurs when allergens are taken up by antigen-presenting cells that migrate to lymph nodes and present the allergen to Tcells, which then proliferate. Some of the new Tcells return to the site of allergen entry into the body, where
Graft and -
-
they produce gamma interferon, which activates macrophages, and tumor necrosis factor, which stimulates an inflammatory response. Mycobacterium tuberculosis, poison ivy Organ Donation Types: Isograft/syngraft: Autograft; Synthetic Graft; Xenograft: Allograft Purposes: Art/Aesthetic; prevention of infection; prevent fluid loss Forms of Graft: skin graft; flap graft; flee graft Pre-op and Post-op Care Recipient Site: free of infection; good vascularization in the area; cleaned aseptically before surgery/ prevent fluid collection on the graft; prevent infection; prevent graft movement; promote adequate circulation in the area Donor Site: celan site; free of infection/ cover dressing during the 1 st 24 hours within mesh gauze until the site is dried up; promote circulation; analgesics; nutrition
Tissue Rejection – healthy defense mechanism of the body First set rejection: recipient receives unmatched skin 2-3 days the body accepts the skin, there is vascularization 6 - 10TH day + lympadenopathy 10 – 14th day + appearance of rejection taking place with the appearance of macrophages and T lymphocytes on the site of transplant 12 – 40th day + necrosis, tissue implanted will now shed off Second set rejection: no vascularization, direct sloughing off tissue Organ Transplantation for end stage or failure and do not respond to conventional therapy Recipient: free of irreversible of infection or malignancy End stage of failure and do not respond to conventional therapy No anatomical problem that would lead to difficulty of transplantation Therapeutic or benefit of the patient Ability of the family to pay costs; age; functional ability; rehabilitation potential; ability to return to work; psychological status; family system, ability to buy post transplantation regimen Donor: cadaver-brain death; no existing disease; no transmissible disease; no malignancy; family with no history of death of unknown causes Types of Rejection: hyper acute; acute; chronic Therapies to prevent Rejection: azaththjioprine; glucocorticoids; ALG
Immunosuppressive
drugs;
cyclosporine;
Summary of Hypersensitivity Reactions Property
Type I Anaphylactic
Type 2 Cytotoxic and Cytolytic
Type 3 Immune Complex
Mediators
IgE, IgG, Baasophils mast cells Drugs, stings
IgG, IgM, complement sytem BT
IgG, IgM
(+) wheal and flare within 30 minutes Secondary to prostaglandin, bradykinin, serotonin, histamine Systemic anaphylaxis, asthma
Not done
Allergens Response to Skin Test Pathophysiolog y and effect
Examples
Soluble agents like drugs Erythema, edema
Type 4 Cell Mediated or Delayed Response T cells, macrophages PTB, Ca Tissue induration
Destruction of cells, RBC
Acute inflammatory reagent
Tissue destruction
ABO incompatibility
Serum sickness
TB, organ donation
DISRUPTIVE INFLAMMATORY RESPONSES COMMUNICABLE DISEASE IN CHILDREN Nursing Process Overview Assessment: History Taking: Local or systemic infection; history of travel; any with animal or animal products; any animal or insect bites; any illnesses that compromises body defenses; what medications taken; vaccination history Clinical Manifestations: 1. Assess for clinical manifestation of infection
2. Obtain specimens of blood, urine, stool, sputum, throat swabbing, nasal secretions, pyrogenic exudates for bacteriologic studies 3. Secure/Assist in securing blood smears or other materials for microscopic studies 4. Assist with spinal aspiration of lumbar tap, BM or any other fluids or tissues for cytologic, serologic or bacteriologic study 5. Carry out appropriate skin tests for specific diagnostic reactions as directed Nursing Diagnosis: 1. Fluid and electrolyte imbalance 2. Altered thermoregulatory status 3. Fever 4. Potential for spread of infection 5. Altered respiratory status 6. Altered elimination status 7. Potential for serious systemic complications 8. Ineffective coping and social isolations 9. Knowledge deficit Planning and Implementation: 1. Implement therapeutic plan to treat infection 2. Ensure hemostasis 3. Measure to prevent cross contamination of infection 4. Prevent overwhelming infection in the immunocompromised patient 5. Relief of symptoms of infection 6. Enhance coping mechanism to promote adaptation Immunization – receiving immunity against a number of dangerous infections. Immunity – ability to combat a particular antigen, ive or active Active Immunity – when the child produces antibodies after the natural invasion of a pathogen Naturally Acquired Active Immunity – ability to produce antibodies rapidly should be specific antigen invade again; lasting. Artificially Acquired Active Immunity – when pathogens are artificially injected into the child by immunization. Should be specific antigen enter again, antibodies are produced against the pathogen that are just as lasting as those produced are in naturally acquired active immunity. ive Immunity – IgG antibodies that a woman possesses, either through immunization or through having a disease are transferred across the placenta to a fetus in utero. Naturally Acquired ive Immunity – fetus does not make antibodies but received them. Artificially Acquired ive Immunity – injection of antibodies made synthetically or obtained from animal serum to the child to give rapid immunity lasting approximately for six weeks.
Immunization Schedule Vaccine
Indication
Age
Dose
BCG (1 dose at birth)
Tuberculo sis
At birth School entrant
1 dose (0.5 ml)
DPT (3 doses) OPV HEP B (3 doses) MEASLES
9 months
Frequenc y 2x
Route Intradermal deltoid
0.5 ml
3x
IM vastus lateralis oral
2 drops
3x
0.5 cc
3x
IM vastus lateralis
0.5 cc
once
Subcutaneo us, deltoid, gluteal
Side effects Pain, fever, local abscess Swelling, fever None Local reaction – swelling, fever Fever, local reaction
EXAMINATION – HIGHER CEREBRAL FUNCTION MEMORY TEST Testing requires alertness and is not possible in a confused or dysphasic patient. IMMEDIATE memory – Digit span – Ask patient to repeat a sequence of 5, 6, or 7 random numbers. RECENT memory – ask patient to describe present illness, duration of hospital stay or recent events in the news. REMOTE memory – ask about events or circumstances of occurring more than 5 years previously. VERBAL memory – ask patient to a sentence or a short story and test after 15 minutes. VISUAL memory – ask patient to objects on a tray and test after 15 minutes. Note: Retrograde amnesia – loss of memory of events leading up to a brain injury or insult. Post traumatic amnesia – permanent loss of memory of events for a period following a head injury. REASONING AND PROBLEM SOLVING Test patient with two-step calculation, e.g. “I wish to buy 12 articles at 7 pence each. How much change will I receive from L1? Ask patient to reverse 3 or 4 random numbers. Ask patient to explain proverbs. Ask patient to sort cards into suits. The examiner must compare patient’s present reasoning ability with expected abilities based on job history and/or schoolwork.
EMOTIONAL STATE Note: Anxiety or excitement Depression or apathy Emotional behavior Uninhibited behavior Slowness of movement or responses Personally type or change COGNITIVE SKILL Listen to language pattern – hesitant - fluent Does the patient understand simple/complex spoken commands? e.g. “Hold up both arms, touch the right ear with the left fifth finger.” Ask the patient to name objects Does the patient read correctly? Does the patient write correctly? Ask the patient to perform numerical calculation, e.g. serial 7 test, where 7 is subtracted serially from 100. Can the patient recognize objects? E.g. ask the patient to select an object from a group.
Dominant hemisphere disorders Expressive dysphasia Receptive dysphasia Receptive dysphasia
Nominal dysphasia Dyslexia Dysgraphia Dyscalculia Agnosia Non- Dominant hemisphere
disorders Note patients ability to find his way around the ward or his home. Can the patient dress himself? Note the patient’s ability to copy a geometric pattern, e.g. ask the patient to forma star with matches or copy a drawing of a cube.
Geographical agnosia Dressing apraxia Constructional apraxia
Mild mental function tests and Functional activity questionnaire are used in the assessment of DEMENTIA
MENTAL BEHAVIOR Level of Consciousness: Alert verbal, painful Drowsy asleep; may
awake, quick, clear mentation, normal response to tactile, stimuli responds to stimulus, may be aroused quickly but easily falls
Obtunded falls back Stuporous painful
yawn frequently, fall asleep during meal or lengthy conversation. can be aroused and responsive, but he’s usually confused and -
to sleep as soon as he is not directly stimulated does not respond spontaneously to environment, vigorous, often stimuli are necessary to arouse the patient. When stimulated, he
move Semi-comatose Comatose some Confusion Apathy Aura flash of
-
but movements are not purposely. Responsive only to deep painful stimulation no response to any stimulation, movement are absent except for muscle reflex contraction state of mental confusion and excitement lack of emotional response a sensory phenomenon that may precede a convulsion, such as light, or ringing bells. HANDOUT IN NEUROLOGIC NURSING
Abberration Decerebrate Denervate drug Contrecoupinjury the
-
NOMENCLATURE deviation from normal structure of behavior deprived of cerebral function to interrupt motor/sensory nerve supply to a party by
-
injection or operation injury to the brain produced on the side opposite that of
Cerebral Concussion brain due to blow
primary injury brain injury resulting from violent jarring of the to the head, fall
Craniotomy Craniectomy Chordotomy the
SURGICAL PROCEDURE surgical opening through the cranium the surgical removal of a part of the skull division of the long tract of the spinal cord, referring usually to antero-lateral pathways that transmit pain
Hypoglycoorrhakia Pleocytosis Xaantochromia -
CSF low sugar in CSF increased WBC in CSF yellowish discoloration of the CSF
Macrocephalous Microcephalous
HEAD having an unusually large head having an unusually small head
-
Cephalococle Cephalhematoma “Foot drop” gait elevates the
-
protrusion of the brain from the cranial cavity subcutaneous swelling containing blood found in the head GAIT due to weakness in dorsiflexing the ankle, the patient affected foot higher than normal and the foot tends to
point Spastic gait and
-
flexion of the knee and hip t is slowly and imperfectly performed; affected leg tends to remain adducted. The patient has to swing the affected leg around (circunduct) since he cannot flex and elevate it. the patient shows loss of arm swing, short-stepped,
Parkinson Gait with the
Ataxic
-
Titubation Festination 1. Propulsion 2. Retropulsion Scissors other Emprosthothonus forehead and
trunk developing a forward list, eventually forcing the patient, with his difficulty in stepping, to have to run forward to “catch up” with the center of gravity, affected arm is characteristically held in semiflexion at the elbow and wrist. patient show either or both of these abnormalities: 1. He cannot accurately place one foot in front of the other and leg movement is jerky and uncoordinated: tends to fall on one side. 2. He may be unable to stabilize his trunk in the vertical posture so that he tends to jerk back and forth (titubation) + Rombryg test (sensory) staggering gait morbid acceleration of gait tendency to push or fall forward in walking walking backward, involuntary short, slow steps, with legs alternately crossing over each POSITION lying with the body in curved and resting upon the feet with face downward. an arched position of the body with the feet and
Opisthotonus head on the floor Pleurothotonus to one side Orthotonus line
downward. associated with spastic weakness, movement is slowed
or bed. titanic spasm in which the body position is arched -
titanic spasm marked by rigidity of the body in a straight MOVEMENTS, COORDINATION, TONE
Coordination complex
-
harmonious action of muscle groups in performing movement inability to perform certain acts or purposeful
Apraxia movements Dyskinesia Akinesia synergia are in
-
Dysmetria
-
-pointings when trying
without motor loss. defect in voluntary movements absence of muscle lack of coordination between muscle groups; movements serial order instead of being made together inability to fix the range of a movement; undershoots or overshoots tendency to veer to one side of tip of nose or finger
Bradykinesia Spasm contraction Fasciculation a single
-
to touch it extreme slowness of movement involuntary, sudden movement or muscular
-
produce localized, incoordinated, involuntary twitching of
Tic of the
-
muscle group while muscles are at rest. coordinated, stereotyped spasmodic muscular contraction
-
face, neck or shoulder muscles that may be involuntary or the result of a habit rhythmic quivering: involuntary movement of a part of the
Tremor body
resulting from the alternate contraction of opposing muscles 1. Coarse Tremors – oscillations are relatively slow (6-7 per sec.) 2. Fine Tremors – rapid, characterized by oscillation of 810 times per second Twitching convulsions quick spasmodic contraction of muscles paroxysm of involuntary muscular contractions and relaxations 1. Clonic movement - one having intermittent contractions, muscles alternately contract and relax 2. Tonic – one which the contractions are maintained for a time which usually draw ts into position of flesion/extension Chorea/Choreiform hallmark of chorea; are purposeless, rapid, jerky usually involving the movements extremities and trunk with facial grimacing, ex. Flexing and extending fingers Ballismus quick jerky shaking movement Hemiballismus quick jerky movement involving half of the body Athetosis repeated involuntary movement of slow, squirming, writhing,
-
twisting type. involuntary movement of the eyeballs resistance all through the ROM resistance of movement at the beginning then, giving in Muscular resistance is characteristically intermittent when
-
muscles are palpated. involuntary muscle movement at rest involuntary movement seen when doing something decreased muscle tone muscular weakness, softness and flabbiness, no motor
-
stiffness of the neck temporary suspension or permanent loss of voluntary
Spastic Paralysis or
-
sensation in a body part involved part of the body is in a state of muscular rigidity
Flaccid Paralysis Paraplegia Hemiplegia Diplegia Quadriplegia Paresis Blepharopthosis
-
Nystagmus Rigidity Spasticity Cogwheel Rigidity the Rest Tremors Intention Tremors Hypotonia Flaccidity response Nuchal rigidity Paralysis motion and
Paresthesia Hyperesthesia Neuralgia Myalgia Agnosia sensation
-
Dysarthria Dysphasia
SENSATION peculiar sensation of numbness, prickling, tingling. unusual sensitivity to pain or sensory stimuli severe Lancination pain along the course of a nerve muscular pain loss of comprehension of audio-v, visual or other 1. Auditory – inability to interpret sounds 2. Optic – inability to interpret images seen 3. Tactile – inability to distinguish objects by using sense of touch is the inability to recognize familiar objects by
Asteriognosis touch or Diplopia Anopsia Homonymous eye Anosmia
tenseness involved part is completely relaxed or limp paralysis of the lower half of the body paralysis of the longitudinal half of the body paralysis of like parts on either side of the body paralysis of the four extremities muscle weakness of partial or incomplete paralysis dropping of the upper eyelid
manipulation double vision loss of vision in one eye Hemianopsialoss of one-half of the field of vision in one -
-
absence of the sense of smell
-
SPEECH AND LANGUAGE difficulty in articulation impairment in speech
Aphasia written
Alexia Agraphua
-
-
Extradural/Epidural frequently Subdural Hemorrhage increasing I
loss or the inability to use or understand spoken or
language; it may exist without intellectual impairment 1. Sensory (receptive aphasia) – inability to comprehend or understand oral or written communication 2. Motor (broca’s) aphasia can’t speak, write although can comprehend 3. Global aphasia – an almost total language loss manifested in minimal response in every phase of language 4. Auditory aphasia – difficulty of understanding spoken word 5. Nominal aphasia – inability to attach meaning to words read inability to read, word blindness inability to express oneself in writing 1. Absolute – complete inability to write 2. Acoustic – inability to write words head 3. Cerebral – inability to express thoughts in writing 4. Motor- inability to write due to muscle coordination 5. Optic – inability to copy words INTRACRANIAL HEMORRHAGE bleeding beneath the cranium and outside the dura, -
hemorrhage between the dura and arachnoid;
develop slowly; personality changes maybe the first noticeable sign Subarachnoid Hemorrhage hemorrhage between the arachnoid and pia mater into CSF NEUROLOGIC SIGNS increasing or widening pulse pressure Decreasing PR Increasing headache Pappil edema Decreased mental awareness Decreased in RR B. Other signs and symptoms which may or may not develop: 1. Vomiting – may or not be projectile 2. Motor deficits – weakness or paralysis of any part of the body 3. Sensory Disturbances of any part of the body 4. Awkwardness – may mean weakness; difficulty or coordination 5. Speech disturbances 6. Convulsion 7. incontinence/retention C. Localizing Symptoms 1. Frontal Lobe – aphasia A. Cardinal symptoms:
Confusion Changes in personality Jacksonian convulsion- convulsion begins in one part of the body and 2. 3. rubber 4. 5.
spread in orderly manner to all of the body parts. Parietal Lobe – convulsion, sensory disturbance, asteriognosis Temporal Lobe – defects in visual field, taste or hearing, smell of burning
Occipital Lobe – visual disturbance Cerebellum Ataxia – muscle coordination especially manifested when voluntary muscular movements are attempted. Tremors, nystagmus, hypotonia 6. Basal Ganglia Athetosis, chorea, hemiballismus, tremor
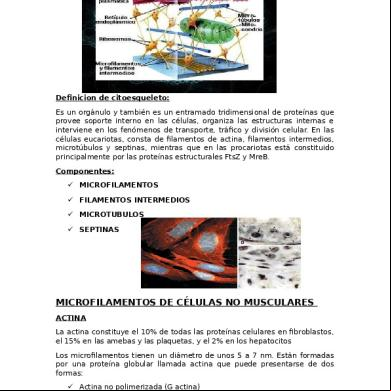
Pathopysiology Cause: excessive alcohol consumption, reduced protein intake, exposure to certain chemicals or infectious schistosomiasis ↓ Episodes of necrosis involving the liver cells ↓ Destroyed liver cells are replaced by scar tissue, the amount of which in time may exceed that of the functioning liver tissue ↓ Early in the disease, the liver is apt to be large and its cells loaded with fat ↓ Later as replacing scar tissue contracts, it becomes small ↓ Also, its surface often becomes rough, bec the scar within it is disposed in coarse bundles, which contract and pull in the capsule at certain points and cause the island of residual normal tissue and of new regenerating liver tissue to project in the little lumps ↓ Liver Enlargement → Activity Intolerance r/t fatigue ↓ Portal Obstruction and Ascites → Ineffective Breathing Pattern r/t ↓ intra- abdominal fluid collection (ascites)
Infection and peritonitis compromised ↓ Gastrointestinal varices altered clotting ↓ Edema compromised ↓ Vit deficiency and anemia ↓ liver Mental deterioration inability of the liver
Body Image Disturbed r/t personal vulnerability → Impaired Skin Integrity r/t immunologic status → Risk for Injury and bleeding r/t Mechanism → Fluid Volume Excess r/t →
regulatory mechanism Nutrition Imbalanced: less than body requirements r/t oral intolerance and Cirrhosis → Risk for acute confusion r/t to detoxify certain enzymes or drugs
Prioritization of Problems: 1. Nutrition Imbalanced: less than body requirements r/t oral intolerance and liver cirrhosis - overt 2. Ineffective Breathing Pattern r/t intra- abdominal fluid collection (ascites) overt 3. Fluid Volume Excess r/t compromised regulatory mechanism - overt 4. Impaired Skin Integrity r/t compromised immunologic status - overt 5. Activity Intolerance r/t fatigue - overt 6. Body Image Disturbed r/t personal vulnerability - overt 7. Risk for Injury and bleeding r/t altered clotting mechanism -covert 8. Risk for acute confusion r/t inability of the liver to detoxify certain enzymes or drugs – covert
Assessment
Pathophysiolog y
Objectives
S: “Nahihirapan akong huminga”
Cause: excessive alcohol consumption, reduced protein intake, exposure to certain chemicals and infectious schistosomiais
STO: After 8 hours of health care interventions pt will be free of dyspnea, cyanosis, w/ ABG’s and vital capacity w/in acceptable range LTO: After 2 weeks of health care intervention pt will establish a normal effective respiratory pattern
O: v/s Temp: 36.7°C BP: 110/60 mmHg PR: 94/min RR: 18/min Conscious: dyspheric Prefers to be in bed Prefers to sleep Assisted w/ ADL by SO Easily fatigued: pallor Appears weak and restless On O2 at 12\LPM/NC Irritable thus changes position once in a while (+) coughing, nonproductive Enlarged
Necrosis of liver cells Destroyed liver cells are replaced by scar tissue Scar tissue exceeds that of functioning liver tissue
Portal obstruction and ascites Ineffective Breathing Pattern
Intervention DX: Monitor respiratory rate, depth and effort
Auscultate breath sounds, noting crackles, wheezes, rhonchi Investigate changes in level of consciousness
Monitor temp. note presence of chills, increased coughing, changes in color/character of sputum Monitor serial ABG’s pulse oximetry, vital capacity measurements, chest x-rays Tx: keep head of bed elevated.
Rationale
Evaluation
Rapid shallow respirations/dyspne smay be present bec. Of hypoxia and or fluid accumulation in abdomen Indicates developing complications, increasing risk of infection
STO: fully met pt is no longer dyspheric and O2 is no longer needed
Changes in mentation may reflect hypoxemia and respiratory failure w/c often accompany hepatic coma.
LTO: fully met if pt will establish a normal or effective respiratory pattern
Indicative of onset infection ex. Pneumonia
Reveals changes in respiratory status developing pulmonary complications
Factors: Pt is very cooperative and willing to participate in any therapy
abdomen (ascites)
Position on sides
A: Ineffective Breathing Pattern r/t Ascites
Provide supplemental o2 as indicated
Conserve pt’s strength by providing rest periods and assisting with activities Change position in every 2 hours Assist with paracentesis or thoracentesis as indicated
Ed Encourage frequent repositioning and deep breathing exercises/cough ing as appropriate Demonstrate
Facilitates breathing by reducing pressure on the diaphragm and minimizes risk of aspiration of secretions Maybe necessary to treat/prevent hypoxia. If respiration/oxygena tion inadequate/ mechanical ventilation maybe required Reduces metabolic and oxygen requirements
Promotes expansion and oxygenation of all areas of the lungs Paracentesis and thoracentesis are performed to remove fluid from the abdominal and thoracic cavities respectively.
with respiratory adjuncts
Aids in lung expansion and mobilizing secretion
Reduces incidence of atelectasis, enhance mobilization of secretions Assessment
Pathophysiolog y
Objectives
S: “wala akong ganang kumain”
Cause: excessive alcohol consumption, reduced protein intake, exposure to certain chemicals and infectious schistosomiais
STO: After 8 hours of health care intervention pt will be able to demonstrate progressive weight gain toward goal with pt appropriate normalization of laboratory values LTO: After 1 month of health care interventions pt will attain desirable weight with optimal
O: v/s Temp: 36.7°C BP: 110/60 mmHg PR: 94/min RR: 18/min Conscious Always in bed and asleep Appears weak and restless Globular or enlarged abdomen
Necrosis of liver cells Destroyed liver cells are replaced by scar tissue Scar tissue
Intervention DX: Measure dietary intake by calorie count Weigh as indicated, compare changes in fluid status, recent weight history, skin fold measurement.
Rationale
Evaluation
Provide information about intake needs or deficiencies It maybe difficult to use weight as indicator of nutritional status in view of edema and ascites. Skin fold measurement are useful in assessing changes in muscle mass and
STO: not met Pt was not able to demonstrate progressive weight gain Factors: Pt doesn’t like to eat because he claims that he is already full Recommendation : Pt needs encouragement NGT insertion
Prominent abdominal veins Tenderness on all quadrants Dull abdomen upon percussion Anorexia: food intolerance Slender body built Increased bowel sounds Oral intolerance (-) nausea and vomiting (-) fever (-) diarrhea
exceeds that of functioning liver tissue Vit deficiency and anemia Nutrient imbalanced: less than body requirement
maintenance of health
Tx: Provide diet high in carbohydrates with protein intake consistent with liver function Elevate head of bed during meals.
Offer smaller, more frequent meals Provide salt substitutes, if allowed, avoid those containing ammonia
Restrict intake of caffeine, gas producing or spicy and excessively hot or cold foods.
subcutaneous fat reserves. Provide calories for energy, sparing protein for healing
Reduces discomfort from abdominal distention and decreases sense of fullness produced by pressure of abdominal contents and ascites in the stomach. Decreases feeling of fullness, bloating Salt substitutes enhance the flavor of foods and aid in increasing appetite ammonia potentiates risk for encephalopathy. Aids in reducing gastric irtrtation/diarrhe
LTO: fully met if pt will attain desirable body weight with optimal maintenance of health Not met: If pt will not attain desirable body weight with optimal maintenance of health
Promote undisturbed rest periods especially before meals Provide oral hygiene before meals aesthetically pleasing setting at mealtime Ed: Suggest soft foods, avoiding roughage if indicated. Recommend cessation of smoking. Encourage pt to eat meals and supplementary feedings
a and abdominal discomfort that may impair oral intake and digestion. Conserving energy reduces metabolic demands on the liver and promotes cellular regeneration. Promotes appetite and sense of wellbeing.
Hemorrhage form esophageal varices may occur in advanced cirrhosis. Reduces excessive gastric stimulation and risk of irritation or bleeding. Encouragement is essential fo the pt w/ anorexia and gastrointestinal discomfort.
NEUROLOGIC INFECTIONS BACTERIAL MENINGITIS - Is an inflammation of the arachnoid, pia, and intervening CSF. The infection spreads throughout the subarachnoid space about the brain and spinal cord and usually involves the ventricles. FACTORS PREDISPOSING TO BACTERIAL MENINGITIS head trauma systemic infection post surgical infection meningeal infection other systemic illness When pathogenic organisms enter the subarachnoid space >inflammatory reaction (CFS clouding, exudates formation, changes in subarachnoid arteries (e.g., engorgement with blood, rapture, thrombosis), and congestion of adjacent tissues. The pia arachnoid becomes thickened and adhesions form, especially in the basal cisterns. Little change occurs in brain structures in the early stages. Almost any bacteria can enter the body causing meningitis o The most common are: Meningoccocus (Neisseria meningitides) Pneumococcus (Streptoccous pneumonia) Haemophilus influence These organisms are often present in nasopharynx. It is not known how they enter the blood stream and the subarachnoid space. Clinical manifestations Headache Prostration Chills Fever N/V
Backpain Stiff neck Generalized seizures Later stage, confused, stuporous, or semicomatose, petechial, or hemorrhagic rash may develop The patient may be irritable at first, but as the infection progresses the sensorium becomes clouded and coma may develop o Signs of meningeal irritation: Nuchal rigidity (rigidity of the neck) Positive finding of Brudzinski’s sign Positive finding of Kernig’s sign MENINGITIS infectious organisms gain access to meninges and subarachnoid spaces (viral, bacterial, yeast) Exudate forms ↓ Meningeal irritation/inflammation ↓ Cortical inflammation ↓ Cerebral edema ↓ Increased I ↓ Vasculitis Increased infection Petechial Hemorrhages Neuritis Hydrocephalos ↓ ↓ ↓ ↓ ↓ Cortical Brain abscess Septic Emboli Cranial nerve Increased Necrosis Septicemias involvement I ↓ ↓ ↓ Adrenal DIC Seizures Compression of Hemorrhage brain structures Hemorrhage
Hypoxia Inadequate perfusion Shock ↓ DEATH
HEADACHES
Is a symptom of an underlying disorder rather than a disease itself. The cause must be identified so that appropriate treatment can be given. Clients often-self treat headaches with OTC medication without prescription. Most headaches do not indicate serious disease however; the nurse should encourage clients with persistent or recurrent headaches to seek neurologic assessment. Serious disorders that typically produce headache include intracranial tumors and infection, bacterial or viral meningitis, head injuries, cerebral hypoxia, severe HPN, acute or chronic diseases of the eye, nose, ear, throat. COMMON TYPES OF HEADACHES I. Migraine - Are paroxysmal disorders characterized by recurrent throbbing headaches - Episodes begin during puberty or ages 20-40 years - They decrease in frequency and severity with advancing years - Affects 5-10% of the population - Women are more susceptible than men are - Occurs at irregular intervals, frequency varies from several times a week to several times a year PATHOPHYSIOLOGY (vascular theory is currently accepted) - Constriction of intracranial vessels > neurologic symptoms - Intense throbbing headache is due to dilation of extracranial and intranial branches of the external carotid artery Psychological factors influence migraine headache o Perfectionist o Fatigue o Excess sleep o Hunger o Refractive errors o Bright light o Surprises o Mental and emotional excitement o Excessive smoking o High altitudes o Drinking alcoholic beverages Certain foods that seem to precipitate migraine episodes, food containing beta-phenylethylamine o Chocolate o Cheese o Citrus fruits o Coffee o Pork products o Dairy products Familial tendency
Oral contraceptive may exacerbate migraines or induce their onset in women previously free from significant headaches. It can occur during menstruation. I.1. Classic or Typical Migraine o Preceded by an aura or prodromal phase in which the client may feel depressed, irritable, restlss, and perhaps anorexic o May experience transient neurologic disturbances (visual phenomena, e.g., flashes of lights, bright spots, distorted vision, diplopia), vertigo, nausea, diarrhea, abdominal pain, paresthesis (numbness of tingling of lips, face, or extremities); may lasts a few minutes or several hours. o Has a “cresendo” quality. It gradually increases in severity until the pain becomes intense and all-encoming.>mild discomfort, >prostrating, throbbing pain >seclusion and lie in bed in a darkened room. o Pain described as dull and boring, pressing, throbbing, or hammering. o Unilateral and may be localized to the front, back, or side of the head, often the temple and eye areas. o Acute migraine episodes lasts 4-6 hours (accompanied by photophobia, N/V, vertigo, tremor, diarrhea, excessive sweating or chilliness). o General sensitivity of all sensory organs and client withdraws from light and sound. o Arteries of the head may become prominent and the amplitude of their pulsation increase, scalp may be very tender, swelling, redness, and excessive tearing of the eyes, and swelling of the nasal mucosa (sometimes accompanied by epistaxis) may occur. I.2. Atypical or Common Migraine o Begins suddenly with or without prodromal symptoms, may be generalized or unilateral, and may or may not be accompanied by N/V. MANAGEMENT: 1. Treat the two phases of migraine, vasoconstriction and vasodilation, analgesics such as acetaminophen may relieve mild H/A. 2. Severe headaches respond to ergot preparations but only if they are taking 30-60 minutes after headache onset. Ergot must be taken before the vessels become rigid from edema in their walls. - Prescribed orally IV or rectally - Once the migraine becomes intense ergot is of little value, stronger analgesic such as codeine sulfate, diphenhydramine hydrochloride (Benadryl). 3. Apply pressure on the common carotid artery and the affected superficial artery. 4. Lying in a dark, quiet room with ice on the back of the neck during acute episodes. 5. Relaxation techniques, bio, or counseling directed at preventing episodes by helping the client understand tensions and resolve major life conflicts. 6. Follow a restrictive diet, avoid food and beverages that contain tyramine and have vasoactive qualities. II. Cluster headaches (Histamine headaches)
-
-
Sometimes classified as a form of migraine. Most clients experiencing cluster headaches do not have a history of migraine headaches. Excruciating painful, unilateral , and tend to occur in clusters. There is usually no aura. Episodes may occur within a few days, weeks, or occasionally months, followed by a remission with no symptoms for months or years. Then the headaches again recur in clusters. Cluster headache may recur at irregular intervals for many years, often related to times of stress anxiety, or emotional upset. Men are affected five times more often than are women. Episodes usually begin in middle life and are often worsened by alcoholic consumption. The mechanism underlying cluster headache is not well understood but is believed to be in vascular origin. These headaches were formerly believed to be caused by sensitivity to histamine. During episode, the client experiences: Excruciating, throbbing, or steady pain arising high in the nostril and spreading to one side of the forehead, around and behind the eye on the affected side. The nose and affected eye water, and the skin reddens on the affected side Nasal congestion and conjunctival infection are common. Intervention is ineffective because of shortness of episodes.
MANAGEMENT: 1. Lying in a dark, quiet room with ice on the back of the neck during acute episodes. 2. Indomethacin (Indocin) medication of choice 3. Tricyclic antidepressant 4. ive care – clients tend to become depressed over their condition and fearful recurrent episodes. Some feel they cannot survive another episode. III. Tension headaches (muscle Contraction Headaches) - Results from the long-sustained contraction of skeletal muscles around the scalp, face, and neck and upper back. - Muscles become tender → client tenses more (primary source of many headaches associated with excessive emotional tension, anxiety and depression.) - Vasodilation of associated cranial arteries may also contribute to muscle irritability and head pain - Begin in adolescence but occur most often in middle age. They may increase significantly in menopause. Pre-menstrual headaches are of this type. - Pain is steady, non-pulsatile ache (unilateral or bilateral) in any region of the head, but more so in the occipital and upper cervical regions and extends diffusely over the top of the head - Onset is gradual, with N/V (late reaction), could also be accompanied by dizziness, tinnitus or lacrimation - Pain could be precipitated by combing the hair, wearing a hat or exposure to cold - Maybe unrelieved for weeks, months or years.
MANAGEMENT: 1. Eliminate source of stimulation (diseased teeth) 2. Psychotherapy for those with prolonged and recurrent muscle tension headaches of psychological in origin 3. Symptomatic relief: massage affected muscles, apply local heat, rest and various relaxation techniques 4. Responds well to a combination of non-narcotic analgesic with an anxiety relieving drug, occasionally a stronger analgesic is needed (e.g., Codeine sulfate).
CLIENT EDUCATION GUIDE
PREVENTING MIGRAINE HEADACHES Many things can trigger a migraine headache. It is important for the client to find out what triggers the headache and avoid the trigger, if possible; if avoidance of the trigger is not possible, the dose of medication can be adjusted. Adjusting Medications During Menstrual Cycles. Menstruation and ovulation may trigger migraines. If medications are taken for migraines, a larger dose may be required during these times. Adjusting Dietary Triggers. Alcohol increases the size of blood vessels (vasodilation) and may increase headache. Some foods contain betaphenlethylamine and should be considered possible triggers. These items include chocolate, cheese, citrus fruits, coffee, pork products and dairy products. The lack of eating may lower blood sugar and may lead to headache. In this case, small frequent meals may avert headaches. Identifying the Role of Stress. Stress may trigger migraines. If stressors cannot be reduced, then medications may need to be increased. Heat intolerance (such as vacationing in warm climates) may increase headaches. Other factors related to stress that might trigger headaches include fatigue, excess sleep, and bright sunlight causing a glare from water, roads, or car hoods.
HEMOPHILIA • • • • • • •
A disorder characterized by impaired coagulation of blood and a tendency to bleed. Hereditary coagulation disorder. both hemophilia A (Factor VIII deficiency) and Hemophilia B (Factor IX deficiency) are inherited as sex linked recessive disorder and are therefore almost exclusive for males. Hereditary and limited to males. X-linked recessive disease – it means that, it is common to males but is being transmitted by females. All daughters of hemophiliacs become carrier. Transmitted by a female trait carrier Absence deficiency or malfunction of any one of clotting factors
TRANSMISSION OF HEMOPHILIA Genotype of parents Carrier+N male N female+Hemophiliac Carrier+hemophiliac
N
Female Carrier
50% 0%
50% 100%
Hemophili ac 0% 0%
0%
50%
50%
COMMON TYPES OF HEMOPHILIA 1. Hemophilia A (Classic Hemophilia) • 80% hemophiliacs • Factor VIII deficiency (anti hemophilic factor)
Male N Hemophilia c 50% 50% 100% 0% 50%
50%
2. Hemophilia B (Christmas Factor) • Factor IX deficiency (Plasma Thromboplastin component) 3. Hemophila C • Factor XI deficiency (Plasma Thromboplastin antecedent) STAGES 1. Mild: clotting factor level 6 to 30% • Bruise easily, tendency to nose/gum bleeding 2. Moderate:2 to 5 % • More frequent bleeding episodes; excessive bleeding after surgery or trauma 3. Severe: 1% or less • Spontaneous bleeding; severe bleeding • Hemarthrosis
MANIFESTATIONS: • Diagnosed usually in infancy or early childhood • History of excessive bleeding into any part of the body sponataneoulsy following trauma • History of excessive bleeding following circumcision and dental extraction • PTT of Hemophilia A and hemophilia B is prolonged • Platelet count and prothrombin time is normal TREATMENT • Replace deficient coagulation factor when bleeding episodes do not respond to local treatment (ice bags, manual pressure or dressing, immobilization, elevation and topical coagulants such as fibrin foam and thrombin) • Since the deficient factors are contained in the plasma, fresh plasma and blood or fresh frozen plasma Is given. • In major hemorrhage, adequate blood levels were difficult to maintain without overloading person’s circulation with large volumes of blood and plasma. • In classic hemophilia, treatment of choice in acute bleeding is infusion of concentrate of antihemophilic factor (Factor VII) • Concentrates prevent circulatory overload and produce fewer adverse effects • Usually people who are being transfused with Factor VIII concentrates are easy to acquire AIDS because donors are not screened that well MANAGEMENT: I. Blood Factor replacement Therapy FFP: all clotting factors present Cryoprecipitate: factor VIII, fibrinogen
Lyophilized factor VIII concentrates Vit. K dependent complex: Factor VIII, IX, XI, prothrombin II. Desmopessin for Mild Hemophilia A It triggers the release of Factor VIII CLOTTING FACTORS 1. Factor I – Fibrinogen 2. Factor II – Prothrombin 3. Factor III – Thromboplastin 4. Factor IV – Calcium 5. Factor V – Proaccelerin, labile factor, accelerator globulin 6. Factor VI – omitted 7. Factor VII – Proconvertin, stabile factor, serum prothrombin conversion accelerator (SPCA) 8. Factor IX – Plasma thromboplastin component (PTC) 9. Factor X - Stuart power factor 10.Factor XI – Plasma Thromboplastin antecedent (PTA) 11.Factor XII – Hageman Factor (HF) 12.Factor XIII – Fibrin Stabilizing Factor Extrinsic System
Intrinsic System
Factor III
Factor XII
Factor VII
Factor XI Factor IX Factor VIII
Scheme of clotting Mechanism
Platelet lysis
Factor X Factor V Calcium Prothrombin
Thrombin
Plasminogen Activator Urokinase Plasminogen
Plasmin
COMMON BLEEDING AND COAGULATION BLOOD TESTS TEST Bleeding time
Clotting time (CT) Prothrombin Time (PT)
Partial Thromboplastin Time (PTT) Activated Partial Thromboplastin (APTT)
DESCRIPTION -Evaluation of vascular platelet factors – the time it takes for a small stab wound to stop bleeding -time required for solid clot to form (less sensitive test than PTT) -indicates rapidity of blood clotting (indicates adequacy of extrinsic coagulation pathways for factors I, II, V, VII and X) -more sensitive test than PT to evaluate adequacy of intrinsic coagulation pathway (Fibrin formation) -modified PTT; more sensitive; quicker to perform, frequently used to monitor heparin therapy and hemoglobin
NORMAL VALUES 2 to 9 minutes
5 to 10 minutes 11 to 16 seconds
60 to 90 seconds
26 to 42 seconds
HYPERTENSION: • Elevated blood pressure • A sustained blood pressure greater than 90 mmHg or a sustained systolic pressure in excess of 140 mmHg is considered to constitute hypertension. • About 90-95 of hypertension is idiopathic and apparently primary (Essential hypertension) • Of the remaining 5-10%, most is secondary to renal disease or less often, to narrowing of the renal artery, usually by an atheromatous plaque (Renovascular hypertension) • Infrequently, secondary hypertension is the result of disease related to the adrenal glands. REGULATION OF NORMAL BLOOD PRESSURE: The magnitude of the arterial blood pressure depends on two hemodynamic variables: a. Cardiac output b. Total peripheral resistance CARDIAC OUTPUT: • Influenced by blood volume, which Is greater dependent on body sodium • Thus, sodium homoestasis is central to blood pressure regulation TOTAL PERIPHERAL RESISTANCE: • Predominantly determined at the level of the arterioles and depends on lumen size, itself dependent on the thickness of the arteriolar wall and the effects of neural and hormonal influences that either constrict or dilate these vessels.
• Normal vascular tone depends on the competition between: a) Vasoconstricting influences Angiotensin II Catecholamines Thromboxane Leukotrienes Endothelin b) Vasodilators: Kinins Prostaglandins Nitric oxide •
•
• • •
Certain metabolic products…. a. Lactic acid b. Hydrogen ions c. Adenosine And hypoxia…can also function as local vasodilators!
GENETIC FACTORS: It is now thought that essential hypertension results from an interaction of genetic and environmental that affect cardiac output or both. ENVIRONMENTAL FACTORS: Environmental factors are thought to contribute to expression of the genetic determinants of increased pressure. Stress, obesity, physical inactivity, and heavy consumption of salt have all been implicated as exogenous factors in hypertension. In both the major pathways for hypertension – primary renal and primary vascular defects – heavy sodium intake augments hypertension. MECHANISMS: • What then are the primary defect in essential hypertension? • Two overlapping pathways are proposed: a. Renal retention of excess sodium The existence of genetic factors that result in reduced renal sodium excretion – in the presence of normal arterial pressure – as the initiating event. Decreased in sodium excretion leads to an increased in fluid volume and a high cardiac output. In the face of an increasing cardiac output, peripheral vasoconstriction occurs as a result of auto regulation to prevent the over perfusion of tissues that would ensue from an increase cardiac output. Auto regulation leads to an increase in peripheral resistance, however, and along with it an elevation of blood pressure.
At the higher setting of blood pressure, enough additional sodium can be excreted by the kidneys to equal intake and prevent fluid retention. Thus, an altered but steady state of sodium excretion is achieved (resetting of pressure natriuresis) but at the expense of stable increases in blood pressure b. Vasoconstriction and vascular hypertrophy Such increased resistance is caused either by factors that induce functional vasoconstriction or by stimuli that induce structural changes in the vessel wall like a. Remodeling b. Hypertrophy c. Hyperplasia of smooth muscle cells Leading to thickened wall and narrowed lumen or by both effects. Vasoconstrictive influences may consist of: 1. Behavioral or neurogenic factors – as exemplified by the reduction of blood pressure achieved by meditation (therelaxation response 2. Increase released of vasoconstrictor agents (eg. Rennin, catecholamines, endothelin) 3. Increased sensitivity of vascular smooth muscle to constricting agents. Such vasoconstrictive influences, if exerted chronically, or repeatedly may themselves cause structural thickening of the resistance vessels, thus perpetuating increased blood pressure. Certain vasoconstrictors (eg. Angiotensin II) also function as growth factors causing smooth muscle hypertrophy, hyperplasia and matrix deposition. Conversely, there is evidence that structural changes in the vessel wall may occur early in the hypertension, preceding rather than strictly secondary to the vasoconstriction. Such evidence has led to a hypothesis that genetic or environmentally induced defects in intracellular signaling in smooth muscle cells affect cell cycle genes and ion fluxes that modulate both smooth cell growth and increased vascular tone resulting in wall thickening and vasoconstriction respectively. SUMMARY: • Essential hypertension is a complex disorder that almost certainly has more than one cause. • It may be initiated by environmental factors – stress, salt intake, estrogens… Which affect the variables that control blood pressure in the genetically predisposed individual. • In established hypertension, both increased cardiac output and increased peripheral resistance contribute to the increased pressure. VASCULAR PATHOLOGY:
• •
Hypertension accelerates atherogenesis and causes structural changes in the walls of blood vessels that potentiate both aortic dissection and cerebral hemorrhage. Hypertension is associated with two forms of small blood vessel disease. a. Hyaline arteriosclerosis b. Hyperplastic arteriosclerosis Both lesions are related to elevations of blood pressure, but other causes may also be involved.
HYALINE ARTERIOSCLEROSIS: • The vascular lesion consist of homogenous, pink hyaline thickening of the walls of arterioles with loss of underlying structural detail and with narrowing of the lumen. • It is believed that the lesions reflect leakage of plasma components across vascular endothelium and increasing extracellular matrix production by smooth muscle cells. • Presumably, the chronic hemodynamic stress of hypertension or a metabolic stress in diabetes accentuates endothelial injury, thus resulting in leakage and hyaline deposition. • The narrowing of the arterial lumens causes impairment of the blood supply to affected organs particularly well exemplified in the kidneys. • Thus, hyaline arteriosclerosis is a major morphologic characteristic of benign nephroscerosis in which the arteriolar narrowing causes diffuse renal ischemia of the kidneys. HYPERPLASTIC ARTERIOSCLEROSIS: • Related to more acute or severe elevation of blood pressure and is therefore characteristic of but not limited to malignant hypertension (diastolic pressure more than 110 mmHg). • This form of arteriolar disease can be identified with the light microscopy by virtue of its onion skin, concentrated laminated thickening of the walls of arterioles with progressive narrowing of the lumens. Note: • The kidneys play a very important role in blood pressure regulation. • Renal dysfunction is essential for the development and maintenance of both essential and secondary hypertension. • The kidney influences both peripheral resistance and sodium homeostasis, and the rennin-angiotensin system appears central to these influences. • Rennin elaborated by the juxtaglomerular cells of the kidney transforms plasma angiotensin to angiotension I. • angiotension I is converted to angiotension II by angiotension converting enzyme (ACE) • angiotension II alters blood pressure by increasing both peripheral resistance and blood volume. • Increasing peripheral resistance is achieved largely by its ability to cause vasoconstriction through direct action on vascular smooth muscle.
• •
• • •
Blood volume is increased by stimulation of aldosterone secretion --- which increases distal tubular reabsorption of sodium and thus, of water. The kidney produces a variety of vasodepressor or antihypertensive substances that presumably counterbalance the vasopressor effects of angiotensin. These include: a. Prostaglandins b. Platelet activating factor c. Urinary kalikrein – kinin system d. Nitric oxide When blood volume is reduced; the GPR falls, this, in turn leads to increased reabsorption of sodium by the proximal tubules in an attempt to conserve sodium and expand blood volume. GFR – independent natriueretic factors, including atrial natriuretic factor (ANF), a peptide secreted by heart atria in response to volume expansion, inhibit sodium reabsorption in distal tubules and cause vasodilation. Abnormalities in these renal mechanisms are implicated in the pathogenesis of secondary hypertension in a variety of renal diseases, but they also play important roles in essential hypertension.
PATHOGENESIS OF ESSENTIAL HYPERTENSION: • Arterial Hypertension occurs when changes develop that after the relationship between blood volume and total peripheral resistance. • In renovascular hypertension, renal artery stenosis causes decreased glomerular flow and pressure in the afferent arteriole of the glomerulos and induces rennin secretion by the juxtaglomerular cells. • This initiates angiotension II induced vasoconstriction --- increased peripheral resistance; through the aldosterone mechanism, --- increased sodium reabsorption and increased blood volume. • In Pheochromocytoma, a tumor of the adrenal medulla, catecholamines produced by tumor cells cause episodic vasoconstriction and thus induce hypertension.
PARKINSON’S DISEASE Brain disorder causing progressive deterioration, with muscle rigidity, akinesia, and voluntary tremors Usual cause of death: aspiration pneumonia One of the most common crippling diseases in the United States
Affects more men than women Occurs in middle age or later Pathophysiology: • Dopaminergic neurons degenerate, causing loss of available dopamine • Dopamine deficiency prevents affected brain cells from performing their normal inhibitory function • Excess excitatory acetylcholine occurs at synapses • Nondopaminergic receptors are also involved • Motor neurons are depressed Causes: • Usually unknown • Exposure to such toxins as manganese dust and carbon monoxide Common Characteristics: Muscle rigidity and tremor Resistance to ive muscle stretching Akinesia and dysarthria and drooling High-pitched, monotonous voice, and loss of posture control Excessive sweating and decreased GI motility Orthostatic hypotension and oily skin and eyes fixed upward Complications: injury from falls; food aspiration; urinary tract infections; skin breakdown Assessment: Insidrous (unilateral pill-roll) tremor, which increases during stress or anxiety and decreases with purposeful movement and sleep Dysphagia Fatigue with activities of daily living (ADLs) Muscle cramps of legs, neck, and trunk Increased perspiration and insomnia, mood changes Treatment: • Small, frequent meals and high-bulk food • Physical therapy and assistive devices to aid ambulation • Medication: Dopamine replacement drugs, anticholinergics, antiviral agents, enzyme-inhibiting agents and tricyclic antidepressants • Surgery used when drug therapy fails • Destruction of ventrolateral nucleus of thalamus New research on the pathogensis of Parkinson’s disease focuses on damage to the substantia nigra from oxidative stress. Oxidative stress is believed to: Alter the brain’s iron content Impair mitochondrial function Alter antioxidant and protective systems Reduce glutathione
Damage lipids, proteins, and deoxyribonucleic acid
Nursing Diagnoses: • Interrupted family processes • Imbalanced nutrition: less than body requirements • Bathing or hygiene self-care deficit • Disturbed body image • Chronic low self-esteem • Constipation • Dressing or grooming self-care deficit • Feeding self-care deficit • Impaired physical mobility, social interaction, verbal communication • Ineffective coping and risk for injury The patient will: Perform ADLs and develop alternative means of communicating Avoid injury and maintain adequate calorie intake Express positive feelings about himself Develop adequate coping behaviors and seek resources Nursing Interventions: • Take measures to prevent aspiration • Protect the patient from injury • Stress the importance of rest periods between activities • Ensure adequate nutrition • Provide frequent warm baths and massage • Encourage the patient to enroll in a physical therapy program • Provide emotional and psychological • Encourage the patient to be independent Monitor: Vital signs, intake and output Drug therapy and adverse reactions to medications Postoperatively: signs of hemorrhage and increased intracranial pressure
MYASTHENIA GRAVIS Abnormal fatigability of striated (skeletal) muscles Sporadic but progressive weakness
Muscle weakness exacerbations by exercise and repetitive movement Muscle weakness improved by anticholinesterase drugs Initial symptoms related to cranial nerves With respiratory system involvement, may be life-threatening Spontaneous remissions in about 25% of patients Occurs at any age Three times more common in women than men Highest in women ages 18 to 25, in men ages, 50 to 60 Transient myasthenia in about 20%of infants born to myasthenic mothers
Pathophysiology: • Blood cells and thymus gland produce antibosies that block, destroy, or weaken neuroreceptors (which transmit nerve impulses) • The result is failure in transmission of nerve impulses at the neuromuscular junction Causes: • Autoimmune disorder associated with the thymus gland • Accompanies other immune and thyroid disorders Common Characteristics: Weak eye closure, ptosis and Diplopia Skeletal muscle weakness; paralysis Complications in respiratory distress, pneumonia, aspiration Assessment: Varying assessment findings Progressive muscle weakness Extreme weakness and fatigue (cardiac symptoms) Ptosis and diplopia (the most common sign and symptom) Difficulty chewing and swallowing Jaw hanging open (especially when tired) and Head bobbing Symptoms milder on awakening worsen as the day progresses Short rest periods that becomes more intense during menses, after emotional stress, after prolonged exposure to sunlight or cold, and with infections
Physical Findings: Sleepy, masklike expression
Drooping jaw Ptosis Decreased breath sounds and tidal volume Respiratory distress and myathenic crisis
Treatment: Plasmapheresis Emergency airway and ventilation management Diet as tolerated Activity as tolerated; exercise may exacerbate symptoms Medication: Anticholinesterase drugs, cortiscosteroids, I.V, immune globulin Surgery: Thymectomy
• •
MULTIPLE SCLEROSIS Progressive demyellination of white matter of brain and spinal cord Characterized by exacerbations and remissions
• • • • •
May progress rapidly, causing death within months Prognosis varies (70% lead active lives with prolonged remissions Highest in women, among people in northern urban areas, in higher socioeconomic groups Family history increases with living in a cold, damp climate Major cause of chronic disability in young adults ages 20 to 40
Pathophysiology: • Sporadic patches of demyelination occur in the central nervous system (CNS), resulting in widespread and varied neurologic dysfunction Causes: • Exact cause unknown • Slowly acting viral infection • An autoimmune response of the nervous system • Allergic response • Events that precede the onset: Emotional distress Overwork Fatigue Pregnancy Acute respiratory tract infections • Generic factors possibly also involved Risk Factors: • Trauma, Anoxia, and toxins • Nutritional deficiencies • Vascular lesions • Anorexia nervosa Common Characteristics: • Dependent on the extent and site of myelin destruction • Sensory impairment • Muscle dysfunction • Bladder and bowel disturbances • Speech problems and fatigue • Complications in injuries from falls, urinary tract infections, constipation, contractures, pressure ulcers and pneumonia •
Multiple Sclerosis (MS)described as:
Elapsing remitting – clear elapses with full recovery lasting disability. Between attacks, the disease doesn’t worsen Primary progressive – steady progression or worsening of the disease from the onset with minor recovery or plateaus Secondary progressive begins as a pattern of clear-cut relapses and recovery but becomes steadily progressive and worsens between acute attacks Progressive relapsing – steadily progressive from the onset but also has clear, acute attacks. Differential diagnosis must rule out spinal cord, multiple small strokes, syphilis or another infection, thyroid disease and chronic fatigue syndrome
Assessment: • Symptoms related to extent and site of myelin destruction, extent of remyelination and adequacy of subsequent restored synaptic transmission • Visual problems and sensory impairment (the 1st signs) • Blurred vision or diplopia • Urinary problems • Emotional lability • Dysphagia • Bowel disturbances (involuntary evacuation or constipation) • Fatigue (typically the most disabling symptom) • Poor articulation • Muscle weakness of the involved area • Spasticity; hyperreflexia • Intention tremor and gait ataxia • Paralysis, ranging from monoplegia to quadriplegia • Nystagmus scotoma • Optic neuritis and Ophthalmoplegia Treatment: General for acute exacerbations, for the disease process and for related signs and symptoms High fluid and fiber intake in case of constipation Frequent rest periods Medications: I.V. steroids followed by oral steroids, immunosuppresants, antimetabolics, alkylating drugs, biological response modifiers Nursing Diagnoses: • Activity intolerance • Interrupted family processes
• • • • • • • • • • • •
Imbalanced nutrition: less than body requirements Ineffective role performances Disturbed thought processes Impaired urinary elimination Chronic low self-esteem Constipation Fatigue Impaired physical mobility Compromised family coping Ineffective coping Deficient knowledge chronic pain Risk for infection and injury The patient will: Perform activities of daily living Remain free from infection Maintain t mobility And range of motion Express feelings of increased energy and decreased fatigue Develop regular bowel and bladder habit Use systems and coping mechanism
Nursing Intervention: • Provide emotional and psychological • Assist with physical therapy program • Provide adequate rest periods • Promote emotional stability • Keep the bedpan or urinal readily available because the need to void is immediate • Provide bowel and bladder training if indicated • ister medications • Monitor: o Response to medications o Adverse drug reactions o Sensory drug reactions o Muscle dysfunction o Energy level o Signs and symptoms of infection o Speech o Elimination patterns vision changes o Laboratory results
AMYOTROPHIC LATERAL SCLEROSI Most common motor neuron disease of muscular atrophy Chronic, progressive and deliberating disease that’s invariably fatal No cure Also known as Lou Gehrig’s disease 3 times more common in men than in women Affects people ages 40 to 70
Pathophysiology: • An excitatory neurotransmitter that accumulates to toxic levels • Motor units that no longer innervate • Progressive degeneration of axons that cause loss of myelin • Progressive degeneration of upper and lower motor neurons • Progressive degeneration of motor nuclei in the cerebral cortex and corticospinal tracts Causes: • Exact cause unknown • 10% of patients with amyotrophic lateral sclerosis (ALS) inherit the disease as an autosomal dominant trait • Virus that creates metabolic disturbances in motor neurons • Immune complexes such as those formed in autoimmune disorders Precipitating factor that cause acute deterioration: • Severe stress, such as myocardial infraction • Traumatic injury • Viral infections • Physical exhaustion Common Characteristics: • Muscle weakness • Atrophy • Fasciculations • Respiratory tract infections • Complications of physical immobility Assessment: Mental function intact
Family history of ALS Asymmetrical weakness 1st noticed in one limb Easy fatigue and easy cramping in the affected muscles Physical Findings: Location of affected motor neurons Severity of the disease Fasciculations in the affected muscles Progressive weakness in muscles of the arms, legs and trunk Brisk and overactive stretch reflexes Difficulty talking, chewing, swallowing and breathing Shortness of breath and occasional drooling Treatment: Rehabilitation May need tube feedings No restrictions : as tolerated Medication: muscle relaxants, dantrolene, Baclofen I.V. or intrathecal istration of thyrotropin-releasing hormone Nursing Diagnoses: Imbaanced nutrition: less than body requirements Anticipatory grieving Anxiety Bathing or hygiene self-care deficit Dressing or grooming self-care deficit Feeding self-care deficit Hopelessness Impaired physical mobility Impaired airway clearance Ineffective breathing pattern Ineffective coping Compromised family coping Deficient knowledge (ALS) Risk for impaired skin integrity Risk for infection The patient will: • Maintain a patent airway and adequate ventilation • Maintain t mobility and range of motion (ROM) • Maintain daily calorie requirements
• •
Seek systems and exhibit adequate coping behaviors Remain free from infections
Nursing Interventions: Provide emotional and psychological Teach about active exercises and ROM exercises Promote independence Teach about meticulous skin care Turn and reposition the patient frequently ister ordered medication Teach how to perform deep-breathing and coughing exercises Provide airway and respiratory management Promote nutrition Teach about swallowing regimens and aspirations precautions Monitor: o Muscle weakness o Respiratory status o Speech o Swallowing ability o Skin integrity o Nutritional status o Response to treatment o Complications o Signs and symptoms of infection •
Modifying the home for a Patient with ALS Guidelines: • Explain basic safety precautions, such as keeping stairs and pathways free from clutter, using nonskid mats in the bathroom and in place of loose throw rugs; keeping stairs well lit; installing handrails in stairwells and the shower, tub and toilet areas and removing electrical and telephone cords from traffic areas. • Discuss the need for rearranging the furniture moving items in or out of patient’s care area, and obtaining such equipment as a hospital bed, a commode, or oxygen equipment. • Recommend devices to ease the patient’s and caregiver’s work such as extra pillows or wedge pillows to help the patient sit up, a draw sheet to help him move up in bed, a lap tray for eating, or a bell for calling the caregiver. • Help the patient adjust to changes in the environment. Encourage independence.
•
Advise the patient to keep suction due to handy to reduce the fear of choking due to secretion accumulation and dysphagia. Teach him to suction himself.
GUILLAIN-BARRE SYNDROME A form of polyneuritis Acute, rapidly progressive, and potentiaaly fatal Three • • •
Phases: Acute – lasting from 1st symptoms, ending in 1 to 3 weeks Plateau – lasting several days to 2 weeks Recovery – coincides with remyelination and axonal process regrowth; extends over 4 to 3 years; recovery possibly not complete
Pathophysiology: Segmented demyclination of peripheral nerves occurs, preventing normal transmission of electrical impulses Sensorimotor nerve roots are affected; autonomic nerve transmission may also be affected Causes: Unknown Virus can cause cell-mediated immunologic attack on peripheral nerves Risk Factors: Surgery Rabies or swine influenza vaccination Viral illness Hodgkin’s or some other malignant disease Lupus erythematosus Common Characteristics: Symmetrical muscle weakness initially in lower extremities and progressing to upper extremities Parethesia Diplegia Dyshagia Hypotonia Areflexia
Complications: Thrombophlebitis Pressure ulcers, contractures and muscle wasting Aspiration and respiratory and cardiac compromise
Assessment: Minor febrile illness 1 to 4 weeks before symptoms Tingling and numbness (paresthesia) in the legs Progression of symptoms to arms, trunk and finally, the face Stiffness and pain in the calves Physical Findings: Muscle weakness (major neurologic sign) Sensory loss, usually in the legs (spreads to arms) Difficulty in taking, chewing and swallowing Paralysis of the ocular, facial and oropharyngeal muscles Loss of position sense Diminishes or absent deep tendon reflexes Diagnostic Procedures: • Cerebrospinal fluid (CSF) analysis may slow a normal white blood cell count, an elevated protein count and in severe disease, increased CSF pressure. Others: • Electromyography may demonstrate repeated firing of the same motor unit instead of widespread sectional stimulation • Nerve conduction studies show marked slowing of nerve conduction velocities Treatment: Primarily ive Possible endocrinal intubation or tracheotomy Volume replacement Plasmapheresis Possible tube feeding with endotracheal intubation Adequate calorie intake Exercise program to prevent contractures I.V. beta-adrenergic blockers and parasympatholytics I.V. immune globulin and possible tracheostomy
Possible gastrotomy or jejunotomy feeding tube insertion Nursing Diagnoses: • Imbalanced nutrition: less than body requirements • Impaired urinary elimination • Anxiety and fear • Impaired gas exchange and impaired physical mobility • Impaired verbal communication and ineffective breathing pattern The patient will: Maintain a patent airway and adequate ventilation Develop alternate means of expressing self Maintain required calorie intake daily Establish routine urinary elimination patterns Maintain t mobility and range of motion (ROM) Nursing Interventions: Establish a means of communication before intubation is required Turn and reposition the patient Encourage coughing and deep breathing Begin respiratory at the first sign of dyspnea Provide meticulous skin care ister ive ROM exercises In case of facial paralysis, provide eye and mouth care Prevent constipation Provide emotional ister medications, as ordered Monitor: o Vital signs o Breath sounds o Arterial blood gas measurements o Level of consciousness o Continual respiratory function o Pulse oximetry o Signs of thrombophlebitis o Signs of urine retention o Response to medications
-
Emotional and spiritual encouragement also is important to the healing process.
7. Side effects can include eating and digestion problems. You may completely lose interest in food during your treatment. - Even if you are not hungry, it is important to keep your protein and calorie intake high. - Doctors have found that patients who eat can better handle their cancers and side effects. - Eat when you are hungry, even when it is not meal time. - Eat several small meals during the day rather than 2 or 3 large meals. - Vary your diet and try new recipes. - If you don’t drink alcohol, ask your doctor if you should avoid alcohol during your treatment. - Keep healthful snacks close by nibbling when you get the urge. Drink milkshakes or prepared liquid supplements between meals. Patient receives a low residue diet to prevent frequent bowel movements. Radiation therapy may cause anorexia which may lead to inadequate nutrition and hydration so small frequent feedings or use of nutritional supplements may be required to maintain adequate nutrition. In radiation therapy, fatigue or malaise also contribute to poor nutritional intake thus planned rest periods may provide relief of fatigue providing increased energy for meal preparation or consumption. Nutrition – to promote retention of nutrients, ister antiemetics as prescribed. Encourage high calorie meals when child is least likely to be nauseated. Praise a child’s effort to eat. Provide foods identified by child as special favorites. Serve easy to swallow food at tolerable temperature. If mucous membrane of mouth, pharynx or esophagus is irradiated, modification of diet to bland, soft, or liquid foods will be necessary; mouth is rinsed frequently with a mild alkaline mouthwash; teeth are gently cleansed with absorbent cotton or gauze rather than the usual brush. Avoids foods that are dry and thick. 8. For lactating mothers undergoing radiation therapy. - Advise pt. not to breastfeed to prevent adverse effects to fetus. - Advise pt. to drink plenty of fluids to prevent dehydration. - Monitor nutritional status. 9. Miscellaneous. - A urinary catheter will be in place (if ordered) and must be inspected frequently to ensure that it drains properly. - Any profuse discharge should be reported immediately to the radiation oncologist or gynecologic surgeon.
-
-
-
-
Observing the patient for temperature elevation, nausea, and vomiting. The symptoms may indicate such complications as infection. Patient teaching includes informing the patient that abdominal fullness, cramping, backache, and the urge to void are normal feelings during therapy. Severe should not occur. Mild opioid agents, muscle relaxants or sedative medications may be helpful. Private room, with private bathroom and facilities Room previously occupied with patients previously treated with radionuclide treatment should not be used until the room has been cleansed and surveyed for residual contamination. Items such as bedpans, urinals and basins if disposable may be disposed of as radioactive waste. If these items are not disposable, they shall be thoroughly washed with soap and running water. Any vomitus, gastric contents collected during the first 24 hours by nasogastric aspiration or excessive sputum should be collected in a waterproof container and held for disposal by radiation safety division personnel. Wearing of lead apron The nurse must deal safety with radioactive body discharges by wearing gloves and in some instances placing excreta in containers for special disposal. For a child receiving radiation therapy Provide ample time to answer questions of children undergoing radiation therapy Advise client to wear loose clothing as skin in the area being treated might become more sensitive to touch. Skin changes: The patient is observed for possible reactions: Slight redness for a brief period Transitory epilation Erythema with temporary sweat gland activity suppression Dry desquamation For large doses or sensitive skin; observe the following: Marked erythema followed by purple discoloration Blister formation and moist desquamation Slow healing, leaving skin atrophied, thin and very sensitive to heat, cold and trauma. Permanent epilation and sweat gland destruction After treatment, the area is gently cleansed with tepid water and patted dry; soap is not used and brisk rubbing is avoided. Alcohol, powders, oils, lotions, creams, ointments, deodorants are not used unless prescribed by the doctor. The site is kept dry and may be covered lightly with smooth cloth/cotton but adhesive tape is contraindicated, used an alternative instead. If larynx is treated with radiation, the patient is closely observed 3-4 days for any difficulty in breathing; edema may develop and occlude airway necessitating prompt intubation or a tracheostomy.
-
Frequent blood cell counts are done because the hemapoetic tissue is extremely sensitive to radiation. with persons with an infection should be avoided especially with respiratory infection because of the patients lowered resistance. Patient should have an extra rest, increased fluid intake and a high calorie, high protein, high vitamin diet. If the patient is allowed to go home, the importance of keeping the appointments for his treatments is stressed. Internal Radiation Therapy: - Patient should receive a simple explanation of the procedure and necessary precautions so he will know what to expect and what is expected of him. - Time is taken to answer his questions and dispel misconceptions. - After implantation, temperature is taken every 4 hours, an increase over 38 degrees is perorted. - Any radioactive material should be handled with a long forceps, never with hands. - All dressings should be checked before disposal. - Patient’s visitors are required to maintain a 3 feet distance from the patient. - Health workers should know the time at which the radioactive implant is to be removed and should have necessary equipment in advance and to remind the person responsible for removal. Nursing responsibilities for the patient receiving radiation therapy
Teletherapy The radiation source is exterior to the tumor such as the use of linear accelerator. 1. Remove all opaque objects such as pins, buttons and hairpins and replace clothing with a gown for body X-rays. 2. Have patient perfectly still; maintain position with the use of foam, plastic, plaster (material) devices and/or variety of other materials that can conform to the patient’s anatomy. 3. Tell the patient there will be no sensation or pain accompanying radiation therapy. 4. Advise the patient that he will be alone in the room for the protection of the technician, but will be in voice . 5. Determine from the physician what has been told to the patient about radiation therapy 6. If series of treatments are to be given, include the patient in the planning phase. Brachytherapy - The radiation source is used for surface, interstitial, or intracavity applications 1. The nurse should inform the patient that some skin reaction can be expected but that varies from patient to patient. 2. Do not apply lotions, ointments, cosmetics, etc. to the site of radiation unless prescribed by the physician. Cornstarch may be used when the skin
is dry and or itchy. Discourage vigorous rubbing or scratching. It may destroy skin cells. Techniques while working with patients undergoing radiation therapy: 1. Put on shoe covers and protective gloves before entering patients room. 2. Work quickly but effectively and courteously. Minimize your time in the room. 3. Note: No matter how long you are in the room, you will not receive a radiation exposure large enough to cause adverse effects. 4. Leave all trash, linens, and food trays in the room 5. After leaving the room, wash your hands. 6. Personnel should not smoke, eat or drink in areas where unencapsulated radio active is used in patient treatment or if the possibilities of contamination of the hands persist. General procedures for obtaining specimens from therapy patients 1. Read the instructions posted in the door. 2. Specimen containers must be labeled with radioactive material labels or tape to identify them as radioactive. 3. Put on a face mask if the patient has a tracheostomy or has symptoms of a respiratory infection. 4. Never use sink for handwashing/ use telephone/ cellphones while in the room. Nursing considerations in external radiotherapy: 1. It is important that the patient receive an explanation of the procedure and precautions. 2. Orient the patient and his family in advance, answer their questions and reassure them that the treatments are well controlled and adequate protection is used. 3. Following the treatment, observe for possible reactions. 4. Instruct and suggest care of the skin 5. Avoid patient to with other persons with infections 6. General ive care applicable to all patients receiving radiotherapy include extra rest, an increase fluid intake and a high calorie, high protein, high vitamin diet 7. When reaction develops, reassure that they are not unexpected and are not an indication of a recurrence or worsening of his cancerous disease. Nursing responsibilities in internal radiotherapy: 1. An explanation to the patient of the procedure and the precautions 2. Place the patient in isolation in a single room and indicate that no visitors are allowed 3. Provide a telephone and radio or television and reading materials 4. In close with patient always wear a lead apron or gown and rubber gloves 5. Wear a monitoring badge which records the amount of radiation received by the patient 6. Visit patient once in a while 7. Nurse should wash hands thoroughly after any with patient and other equipment
8. Linens, dishes, syringes, needles and other treatment equipment are monitored before being returned. For infants and children - No cream, no lotion should be applied to radiation areas until the treatment series is completed. - If creams contain any metal, these could distort or interfere with the entrance of radiation. - If the head will be irradiated, a dental consult may be suggested. This can slow healing of a tooth extraction. During treatment: - Require them to be still for a period of time possibly on an uncomfortable table. - Assure patients and the child that during the treatment, just as there is no sensation from x-ray exposure, the child may will experience no sensation from radiation exposure. - Infants are usually prescribed a sedative or conscious sedation before therapy to ensure that they be still during the procedure. - To make this approach affective, keep the child fairly active early in the day and introduce activities after the sedative is istered. After treatment: - If head is involved in therapy, alopecia (hair loss) may result. - Radiation to the head may reduce salivary gland function, leading to a constantly dry mouth. - Tooth growth may be halted due to root therapy. - Radiation to bone marrow may depress blood cell and platelet production. - Children undergoing radiation therapy need their leukocytes and platelet counts monitored periodically for changes. For clients undergoing radiation: - Clients with radioactive implants are a source of radiation to the immediate environment. - The nurse who is in close with such clients also needs to wear a lead apron. - Nurses must deal safely with radioactive body discharges by wearing gloves and in some instances placing excreta in containers for special disposal. - The nurse must wash gloved hands well before and after removing the gloves and placed contaminated materials in a special containers for special disposal. - Nurses must make sure they understand treatment and the precautions they need to take. Often such clients are restricted to bed or to a confined area to protect others. - These clients need emotional to deal with the precautions and will likely accept treatments and precautions better when they know what will happen, when and why. - Exposure of the reproductive organs of mice and rabbits to X rays has caused gene mutations that resulted in malformed offsprings and geneticist believe that comfortable effects can occur in humans.
-
Knowing these, great care is taken to protect both the nurse and patient from unnecessary exposure.
-
Chemotherapy and radiation therapy: knowledge of the appropriate routes, doses and reactions is required. Infection control: nurses must be aware of standard infection control precautions. Nausea and vomiting are most likely to occur when the radiation dose is high or if the abdomen or another part of the digestive tract is irradiated. Sometimes nausea and vomiting occur after radiation to other regions, but in these cases the symptoms usually disappear within a few hours after treatment. Nausea and vomiting can be treated with antacids, Compazine, Tigan or Zafran. Fatigue frequently starts after the 2nd week therapy and may continue until about 2 weeks after the therapy is finished. Patients may need help to limit their activities, take naps and get extra sleep at night.
-
-
Nursing Diagnoses and its Nursing Interventions
-
Nursing Diagnosis: Impairment of skin integrity due to irradiation Nurisng interevntions: - For patients with xerostomia undergoing irradiation - Patient education - Nursing care involves assesing the physical and emotional aspects of the patient before, during and after a course of head and neck irradiation, and providing interventions, education and . - During radiation therapy, the patient should be very gentle with the skin in the treatment area. This nurses can suggest the following: Avoid irritatitng treated skin. When washing, use only lukewarm water and mild soap, pat dry. Do not wear tight clothing over the area. Do not rub, scrub or scratch the skin in the treatment area. Avoid putting anything that is hot or cold, such as heating pad or ice packs on treagted skin. Ask the doctor or nurse to recommend skin care products that will not cause skin irritation. Do not use any powders, creams, perfumes, deodorants, body oils, ointments, lotions or home remedies in the treatment area while you’re being treated and for several weeks afterward unless approved by the doctor. Do not apply skin lotion within 2 hours of treatment. Avoid exposing the radiated area to the sun during treatment, after is over, ask the doctor or nurses how long you should continue to take extra precautions in the sun. Avoid extremes of temperature Avoid rough and tight garments. Avoid rubbing or scratching the area the nurse needs to explain that during treatment, the patient must stay in absolute bedrest.
-
Nurses should know also that over exposure to radiation may include burning and scarring of the skin or lungs; a tendency to develop cataracts; a tendency to develop cancer; to destroy blood producing tissue.
-
Use only luke warm water and mild soap. Just let water run over the treated area. Do not rub. Do not wear tight clothing over the treatment area. Try not to rub, scrub or scratch any sensitive spots. Avoid exposing the area to the sun during treatment and for at least 1 year after the treatment is completed. If you expect to be in the sun for more than a few minutes, wear protective clothing and sunscreen. Ask your doctor or nurse ing sunscreen lotions. Wash the irritated area gently each day with sitter water alone on a mild soap and water. Use your hand rather than a washcloth to be more gentle. Rinse soap thoroughly from your skin. Take care not to remove the markings that indicate exactly where the beam of radiation is to be focused. Dry the irradiated area with potting motions rather than rubbing motions, using a clean, soft towel Use no powders, ointments, lotions, or creams on your skin at the radiation site unless they are prescribed by your radiologist. Wear soft clothing over the skin at the radiation site. Avoid exposure of the irradiated area to the sun. A void heat exposure. Mild erythema to moist desquamation similar to appearance to a second-degree burn. The nurse assesses the patient’s skin, nutritional status and general feeling of well being. The skin and oral mucosa are assesses frequently for changes. The skin is protected from irritation and the patient is instructed to avoid using ointments, lotion or powder on the area. Pressure is avoided by avoiding tight clothing’s and prolonged lying on the area of treatment. No hot or cold is applied on the site and must be protected from direct sunlight. If itching and irritation accompanying erythema, you may suggest application of plain calamine lotion without phenol; or cornstarch. • Dryness and pruritus may occur at an accumulated dose of 2000 to 28000 Cgy (1.2) and is caused by obliteration of sebaceous glands within the field. • This is an acute phenomenon that correlates with the depletion of actively proliferating basal cells in the epidermal layer of the skin, a fixed percentage of which die with each dose fraction of irradiation. • Remaining basal cells are stimulated and their cell cycle shortened. • Subsequent peeling of the skin is defined as dry desquamation. • The skin becomes dry and patient may notice itching and burning sensations.
-
•
Dry skin is susceptible to further injury through scratching and/or formation of fissures – augmenting the risk of infection and tissue necrosis.
Nursing Diagnosis: Potentials for infection due to bone marrow depression Nursing Intervention: - Monitor blood counts weekly. - Teach person to avoid infection by frequent handwashing and good nutrition, hygiene and good habits. - Teach persons signs of infection to report to physician. Nursing Diagnosis: Potential for bleeding due to BM depression: Nursing Interventions: - Monitor platelet counts weekly - Teach person to avoid physical trauma and aspirin while platelets are low - Teach person signs of hemorrhage to report to physician - Monitor stool, integument for signs of hemorrhage - Use direct pressure over injection sites until bleeding stops Nursing Diagnosis: Activity intolerance due to anemia Nursing intervention: - Discuss fatigue and its causes with person - Encourage good nutrition and plenty of rest Nursing Diagnosis: Alteration in Nutrition: Less than body requirements due to anemia Nursing intervention: - Monitor diet for efficient calories - dietitian if indicated - Monitor weight weekly or daily - Assess person’s understanding of nutrition and teach as necessary Nursing Diagnosis: Alteration in mucous membranes due to irradiation Nursing interventions: - Monitor oral cavity daily - Encourage bland diet, no smoking, no alcohol - Good oral hygiene and saline rinses every 2 hours while awake may help - Ensure professional dental care - Avoid foods that are dry and thick Care of the teeth, gums, mouth and throat - Avoid spices and coarse foods such as raw vegetables, dry crackers and nuts - Do not eat or drink very hot foods - Do not smoke, chew tobacco or drink alcohol because tobacco and alcohol can further irritate mouth sores. - Stay away from sugary foods and snacks. - Ask your doctor or nurse to recommend a good mouthwash. The alcohol content in some mouthwashes has a drying effect on mouth tissues. - Sip cool drinks often throughout the day. - Eat or chew sugar free candy or gum to help keep your mouth moist
- Moisten food with gravies and sauces to make eating easier. - Gentle oral hygiene is essential to remove debris, prevent irritation and promote healing Mucositis: do not remove membrane Nursing Diagnosis: Alteration in bowel elimination: diarrhea due to irradiation Nursing interventions: - Monitor stool - Give low residue diet/antidiarrhea medication as prescribed. Nursing Diagnosis: Alteration in comfort and vomiting due to irradiation Nursing interventions: - Plan rest periods before and after meals - ister antiemetics as prescribed - Monitor fluids and electrolytes Nursing Diagnosis: Alteration in comfort: headache due to irradiation Nursing Interventions: - Monitor pain - ister analgesics as prescribed Nursing Diagnosis: Disturbance in self concept due to alopecia Nursing interventions: - Encourage verbalization of feelings - Suggest use of wigs, scarf’s, hats, etc - Instruct person on hair care Nursing Diagnosis: Alteration in urinary elimination patterns due to irradiation Nursing interventions: - Monitor urine for blood - Monitor for dysuria or urinary frequency - Encourage fluid intake Nursing Diagnosis: Social isolation due to irradiation Nursing Interventions: - Explain and discuss irradiation precaution - Encourage telephone calls - Suggest television, radio or tape player - Stop by door to say “hello”
HYPERSENSITIVITY REACTIONS
• •
Exaggerated or inappropriate response to specific antigen Anaphylaxis, allergies, transfusion reactions, graft rejections
TYPE I – Anaphylactic / Immediate Hypersensitivity Reaction Common antigens: Insect bites, drugs, food, pollen, x-ray contrast medium Signs and Symptoms: Urticaria(hives) caused by foods- eggs, fish , nuts, drugs Atopic allergies – less severe and more common form seen in about 15% of the population. Atopy means inherited hypersensitivity. Common Antigens include: Inhalants – dust, pollens, mold spore, animal dander ants – fibers in wool, fur, nylon, plant oils, osaps, cosmetics, perfumes, hair dyes, nickel in jewelry, clothings, occupational chemicals, changes in temperature and stress Pathophysiology: IgE attach to the surface of mast cells and basophils providing a site for allergens to bond the cells. This causes the cells to releases vasoactive substances including histamine leading to: 1. Constriction of smooth muscles in the bronchi – bronchospasm 2. Increase in vascular permeability – urticaria(hives or tissue edema 3. Increase in mucus secretions – hay fever and asthma Symptoms: wheezing, sneezing, rhinitis with conjunctivitis; urticaria, angioedema, rash: diarrhea; fever, malaise, t pains, hematopoietic suppression, anaphylaxis Sensitizing Dose – initial with allergen that triggers the synthesis of specific antiallergenic IgE antibodies Shocking, Challenging Dose – subsequent with allergen, indi exhibits the symptoms of Type I Nursing Process: Assessment – history taking Diagnostic Test – skin test, radioallergosorbent test, one-week food diary test Nursing Diagnosis: Alerted health maintenance; Knowledge deficit Implementation: 1. Prevent anaphylactic reaction - Epinephrine; Benadryl; aminophylline, tracheal intubation; shock therapy 2. Allergen immunotherapy 3. Control the environment – house dust; animal dander; pollens; fungus 4. Facilitate learning – remind physician of allergy if new medications are prescribed; read all labels of nonprescription drugs before taking the new drug; examine all labels of new prepared foods for presence of allergens; avoid eating unknown foods when travelling; use non allergenic soaps and cosmetics – coat nickel containing jewelry with clean nailpolish; use gloves to handle allergen; report side effects of prescribed medication
TYPE II – Cytotoxic Hypersensitivity
•
•
Caused by antibodies (IgG and IgM) directed against antigens on a person’s red blood cells, lymphocytes or platelets or tissue cells. The reaction of antibodies and antigens usually leads to activation of the complement system. Damage cells by causing lysis as in compatible blood transfusion reactions
Types of Transfusion Reactions: 1. Acute hemolytic Reaction/hemolytic transfusion reaction - Infusion of ABO incompatible with blood, RBCs or components containing 10 ml or more RBC’s antibodies in the recipients plasma attach to the antigens on transfused RBC’S ---RBC destruction. Chills, fever, low back pain, flushing, tachycardia, tachypnea, hypotension, vascular collapse, hemoglobinuria, bleeding, ARF, shock, cardiac arrest, death 2. Febrile, Non Hemolytic ( most common) - Sensitization to donor’s WBC’s, platelets or plasma proteins - Sudden chills and fever, headache, flushing, anxiety, muscle pain 3. Mild Allergic reaction involves sensitivity to foreign plasma proteins - Flushing, itching, urticaria 4. Anaphylactic reaction - Infusion of IgA protein to IgA deficient recipient who has developed IgA antibody - Anxiety, urticaria, wheezing, tightness and pain chest, difficulty swallowing, progressing to cyanosis, shock and possible cardiac arrest 5. Delayed hemolytic reaction - An amnestic immune response that occurs 7-14 days after transfusion. Sensitization to RBC antigen not ABO system - Fever, chills, back pains, jaundice, anemia, hemoglobinuria 6. Graft-versus-Host Disease_Pt. - Immunodeficient person receives lymphocytes begin to reject cells 4-30 days after the transfusion. - Anorexia, nausea, diarrhea, high fever, rash, stomatitis, liver dysfunction Prevention of transfusion Reaction: Accurate laboratory testing; careful blood istration TYPE III – Hypersensitivitis/Immune Complex - Involves antigens, antibodies (IgG and IgM) and the complement system. When certain ratios of antigen to antibody occur, the immune complexes are small enough to escape phagocytosis, but they become trapped in the basement membrane under the endothelium of blood vessels, where they activate complement and cause inflammation - Glomerulonephritis and rheumatoid arthritis - Antihistamines and salicylates; steroids – prednisone; epinephrine TYPE IV – Cell mediated or Delayed Hypersensitivity Reaction - Usually appears 12-72 hours after exposure to an allergen. Occurs when allergens are taken up by antigen-presenting cells that migrate to lymph nodes and present the allergen to Tcells, which then proliferate. Some of the new Tcells return to the site of allergen entry into the body, where
Graft and -
-
they produce gamma interferon, which activates macrophages, and tumor necrosis factor, which stimulates an inflammatory response. Mycobacterium tuberculosis, poison ivy Organ Donation Types: Isograft/syngraft: Autograft; Synthetic Graft; Xenograft: Allograft Purposes: Art/Aesthetic; prevention of infection; prevent fluid loss Forms of Graft: skin graft; flap graft; flee graft Pre-op and Post-op Care Recipient Site: free of infection; good vascularization in the area; cleaned aseptically before surgery/ prevent fluid collection on the graft; prevent infection; prevent graft movement; promote adequate circulation in the area Donor Site: celan site; free of infection/ cover dressing during the 1 st 24 hours within mesh gauze until the site is dried up; promote circulation; analgesics; nutrition
Tissue Rejection – healthy defense mechanism of the body First set rejection: recipient receives unmatched skin 2-3 days the body accepts the skin, there is vascularization 6 - 10TH day + lympadenopathy 10 – 14th day + appearance of rejection taking place with the appearance of macrophages and T lymphocytes on the site of transplant 12 – 40th day + necrosis, tissue implanted will now shed off Second set rejection: no vascularization, direct sloughing off tissue Organ Transplantation for end stage or failure and do not respond to conventional therapy Recipient: free of irreversible of infection or malignancy End stage of failure and do not respond to conventional therapy No anatomical problem that would lead to difficulty of transplantation Therapeutic or benefit of the patient Ability of the family to pay costs; age; functional ability; rehabilitation potential; ability to return to work; psychological status; family system, ability to buy post transplantation regimen Donor: cadaver-brain death; no existing disease; no transmissible disease; no malignancy; family with no history of death of unknown causes Types of Rejection: hyper acute; acute; chronic Therapies to prevent Rejection: azaththjioprine; glucocorticoids; ALG
Immunosuppressive
drugs;
cyclosporine;
Summary of Hypersensitivity Reactions Property
Type I Anaphylactic
Type 2 Cytotoxic and Cytolytic
Type 3 Immune Complex
Mediators
IgE, IgG, Baasophils mast cells Drugs, stings
IgG, IgM, complement sytem BT
IgG, IgM
(+) wheal and flare within 30 minutes Secondary to prostaglandin, bradykinin, serotonin, histamine Systemic anaphylaxis, asthma
Not done
Allergens Response to Skin Test Pathophysiolog y and effect
Examples
Soluble agents like drugs Erythema, edema
Type 4 Cell Mediated or Delayed Response T cells, macrophages PTB, Ca Tissue induration
Destruction of cells, RBC
Acute inflammatory reagent
Tissue destruction
ABO incompatibility
Serum sickness
TB, organ donation
DISRUPTIVE INFLAMMATORY RESPONSES COMMUNICABLE DISEASE IN CHILDREN Nursing Process Overview Assessment: History Taking: Local or systemic infection; history of travel; any with animal or animal products; any animal or insect bites; any illnesses that compromises body defenses; what medications taken; vaccination history Clinical Manifestations: 1. Assess for clinical manifestation of infection
2. Obtain specimens of blood, urine, stool, sputum, throat swabbing, nasal secretions, pyrogenic exudates for bacteriologic studies 3. Secure/Assist in securing blood smears or other materials for microscopic studies 4. Assist with spinal aspiration of lumbar tap, BM or any other fluids or tissues for cytologic, serologic or bacteriologic study 5. Carry out appropriate skin tests for specific diagnostic reactions as directed Nursing Diagnosis: 1. Fluid and electrolyte imbalance 2. Altered thermoregulatory status 3. Fever 4. Potential for spread of infection 5. Altered respiratory status 6. Altered elimination status 7. Potential for serious systemic complications 8. Ineffective coping and social isolations 9. Knowledge deficit Planning and Implementation: 1. Implement therapeutic plan to treat infection 2. Ensure hemostasis 3. Measure to prevent cross contamination of infection 4. Prevent overwhelming infection in the immunocompromised patient 5. Relief of symptoms of infection 6. Enhance coping mechanism to promote adaptation Immunization – receiving immunity against a number of dangerous infections. Immunity – ability to combat a particular antigen, ive or active Active Immunity – when the child produces antibodies after the natural invasion of a pathogen Naturally Acquired Active Immunity – ability to produce antibodies rapidly should be specific antigen invade again; lasting. Artificially Acquired Active Immunity – when pathogens are artificially injected into the child by immunization. Should be specific antigen enter again, antibodies are produced against the pathogen that are just as lasting as those produced are in naturally acquired active immunity. ive Immunity – IgG antibodies that a woman possesses, either through immunization or through having a disease are transferred across the placenta to a fetus in utero. Naturally Acquired ive Immunity – fetus does not make antibodies but received them. Artificially Acquired ive Immunity – injection of antibodies made synthetically or obtained from animal serum to the child to give rapid immunity lasting approximately for six weeks.
Immunization Schedule Vaccine
Indication
Age
Dose
BCG (1 dose at birth)
Tuberculo sis
At birth School entrant
1 dose (0.5 ml)
DPT (3 doses) OPV HEP B (3 doses) MEASLES
9 months
Frequenc y 2x
Route Intradermal deltoid
0.5 ml
3x
IM vastus lateralis oral
2 drops
3x
0.5 cc
3x
IM vastus lateralis
0.5 cc
once
Subcutaneo us, deltoid, gluteal
Side effects Pain, fever, local abscess Swelling, fever None Local reaction – swelling, fever Fever, local reaction
EXAMINATION – HIGHER CEREBRAL FUNCTION MEMORY TEST Testing requires alertness and is not possible in a confused or dysphasic patient. IMMEDIATE memory – Digit span – Ask patient to repeat a sequence of 5, 6, or 7 random numbers. RECENT memory – ask patient to describe present illness, duration of hospital stay or recent events in the news. REMOTE memory – ask about events or circumstances of occurring more than 5 years previously. VERBAL memory – ask patient to a sentence or a short story and test after 15 minutes. VISUAL memory – ask patient to objects on a tray and test after 15 minutes. Note: Retrograde amnesia – loss of memory of events leading up to a brain injury or insult. Post traumatic amnesia – permanent loss of memory of events for a period following a head injury. REASONING AND PROBLEM SOLVING Test patient with two-step calculation, e.g. “I wish to buy 12 articles at 7 pence each. How much change will I receive from L1? Ask patient to reverse 3 or 4 random numbers. Ask patient to explain proverbs. Ask patient to sort cards into suits. The examiner must compare patient’s present reasoning ability with expected abilities based on job history and/or schoolwork.
EMOTIONAL STATE Note: Anxiety or excitement Depression or apathy Emotional behavior Uninhibited behavior Slowness of movement or responses Personally type or change COGNITIVE SKILL Listen to language pattern – hesitant - fluent Does the patient understand simple/complex spoken commands? e.g. “Hold up both arms, touch the right ear with the left fifth finger.” Ask the patient to name objects Does the patient read correctly? Does the patient write correctly? Ask the patient to perform numerical calculation, e.g. serial 7 test, where 7 is subtracted serially from 100. Can the patient recognize objects? E.g. ask the patient to select an object from a group.
Dominant hemisphere disorders Expressive dysphasia Receptive dysphasia Receptive dysphasia
Nominal dysphasia Dyslexia Dysgraphia Dyscalculia Agnosia Non- Dominant hemisphere
disorders Note patients ability to find his way around the ward or his home. Can the patient dress himself? Note the patient’s ability to copy a geometric pattern, e.g. ask the patient to forma star with matches or copy a drawing of a cube.
Geographical agnosia Dressing apraxia Constructional apraxia
Mild mental function tests and Functional activity questionnaire are used in the assessment of DEMENTIA
MENTAL BEHAVIOR Level of Consciousness: Alert verbal, painful Drowsy asleep; may
awake, quick, clear mentation, normal response to tactile, stimuli responds to stimulus, may be aroused quickly but easily falls
Obtunded falls back Stuporous painful
yawn frequently, fall asleep during meal or lengthy conversation. can be aroused and responsive, but he’s usually confused and -
to sleep as soon as he is not directly stimulated does not respond spontaneously to environment, vigorous, often stimuli are necessary to arouse the patient. When stimulated, he
move Semi-comatose Comatose some Confusion Apathy Aura flash of
-
but movements are not purposely. Responsive only to deep painful stimulation no response to any stimulation, movement are absent except for muscle reflex contraction state of mental confusion and excitement lack of emotional response a sensory phenomenon that may precede a convulsion, such as light, or ringing bells. HANDOUT IN NEUROLOGIC NURSING
Abberration Decerebrate Denervate drug Contrecoupinjury the
-
NOMENCLATURE deviation from normal structure of behavior deprived of cerebral function to interrupt motor/sensory nerve supply to a party by
-
injection or operation injury to the brain produced on the side opposite that of
Cerebral Concussion brain due to blow
primary injury brain injury resulting from violent jarring of the to the head, fall
Craniotomy Craniectomy Chordotomy the
SURGICAL PROCEDURE surgical opening through the cranium the surgical removal of a part of the skull division of the long tract of the spinal cord, referring usually to antero-lateral pathways that transmit pain
Hypoglycoorrhakia Pleocytosis Xaantochromia -
CSF low sugar in CSF increased WBC in CSF yellowish discoloration of the CSF
Macrocephalous Microcephalous
HEAD having an unusually large head having an unusually small head
-
Cephalococle Cephalhematoma “Foot drop” gait elevates the
-
protrusion of the brain from the cranial cavity subcutaneous swelling containing blood found in the head GAIT due to weakness in dorsiflexing the ankle, the patient affected foot higher than normal and the foot tends to
point Spastic gait and
-
flexion of the knee and hip t is slowly and imperfectly performed; affected leg tends to remain adducted. The patient has to swing the affected leg around (circunduct) since he cannot flex and elevate it. the patient shows loss of arm swing, short-stepped,
Parkinson Gait with the
Ataxic
-
Titubation Festination 1. Propulsion 2. Retropulsion Scissors other Emprosthothonus forehead and
trunk developing a forward list, eventually forcing the patient, with his difficulty in stepping, to have to run forward to “catch up” with the center of gravity, affected arm is characteristically held in semiflexion at the elbow and wrist. patient show either or both of these abnormalities: 1. He cannot accurately place one foot in front of the other and leg movement is jerky and uncoordinated: tends to fall on one side. 2. He may be unable to stabilize his trunk in the vertical posture so that he tends to jerk back and forth (titubation) + Rombryg test (sensory) staggering gait morbid acceleration of gait tendency to push or fall forward in walking walking backward, involuntary short, slow steps, with legs alternately crossing over each POSITION lying with the body in curved and resting upon the feet with face downward. an arched position of the body with the feet and
Opisthotonus head on the floor Pleurothotonus to one side Orthotonus line
downward. associated with spastic weakness, movement is slowed
or bed. titanic spasm in which the body position is arched -
titanic spasm marked by rigidity of the body in a straight MOVEMENTS, COORDINATION, TONE
Coordination complex
-
harmonious action of muscle groups in performing movement inability to perform certain acts or purposeful
Apraxia movements Dyskinesia Akinesia synergia are in
-
Dysmetria
-
-pointings when trying
without motor loss. defect in voluntary movements absence of muscle lack of coordination between muscle groups; movements serial order instead of being made together inability to fix the range of a movement; undershoots or overshoots tendency to veer to one side of tip of nose or finger
Bradykinesia Spasm contraction Fasciculation a single
-
to touch it extreme slowness of movement involuntary, sudden movement or muscular
-
produce localized, incoordinated, involuntary twitching of
Tic of the
-
muscle group while muscles are at rest. coordinated, stereotyped spasmodic muscular contraction
-
face, neck or shoulder muscles that may be involuntary or the result of a habit rhythmic quivering: involuntary movement of a part of the
Tremor body
resulting from the alternate contraction of opposing muscles 1. Coarse Tremors – oscillations are relatively slow (6-7 per sec.) 2. Fine Tremors – rapid, characterized by oscillation of 810 times per second Twitching convulsions quick spasmodic contraction of muscles paroxysm of involuntary muscular contractions and relaxations 1. Clonic movement - one having intermittent contractions, muscles alternately contract and relax 2. Tonic – one which the contractions are maintained for a time which usually draw ts into position of flesion/extension Chorea/Choreiform hallmark of chorea; are purposeless, rapid, jerky usually involving the movements extremities and trunk with facial grimacing, ex. Flexing and extending fingers Ballismus quick jerky shaking movement Hemiballismus quick jerky movement involving half of the body Athetosis repeated involuntary movement of slow, squirming, writhing,
-
twisting type. involuntary movement of the eyeballs resistance all through the ROM resistance of movement at the beginning then, giving in Muscular resistance is characteristically intermittent when
-
muscles are palpated. involuntary muscle movement at rest involuntary movement seen when doing something decreased muscle tone muscular weakness, softness and flabbiness, no motor
-
stiffness of the neck temporary suspension or permanent loss of voluntary
Spastic Paralysis or
-
sensation in a body part involved part of the body is in a state of muscular rigidity
Flaccid Paralysis Paraplegia Hemiplegia Diplegia Quadriplegia Paresis Blepharopthosis
-
Nystagmus Rigidity Spasticity Cogwheel Rigidity the Rest Tremors Intention Tremors Hypotonia Flaccidity response Nuchal rigidity Paralysis motion and
Paresthesia Hyperesthesia Neuralgia Myalgia Agnosia sensation
-
Dysarthria Dysphasia
SENSATION peculiar sensation of numbness, prickling, tingling. unusual sensitivity to pain or sensory stimuli severe Lancination pain along the course of a nerve muscular pain loss of comprehension of audio-v, visual or other 1. Auditory – inability to interpret sounds 2. Optic – inability to interpret images seen 3. Tactile – inability to distinguish objects by using sense of touch is the inability to recognize familiar objects by
Asteriognosis touch or Diplopia Anopsia Homonymous eye Anosmia
tenseness involved part is completely relaxed or limp paralysis of the lower half of the body paralysis of the longitudinal half of the body paralysis of like parts on either side of the body paralysis of the four extremities muscle weakness of partial or incomplete paralysis dropping of the upper eyelid
manipulation double vision loss of vision in one eye Hemianopsialoss of one-half of the field of vision in one -
-
absence of the sense of smell
-
SPEECH AND LANGUAGE difficulty in articulation impairment in speech
Aphasia written
Alexia Agraphua
-
-
Extradural/Epidural frequently Subdural Hemorrhage increasing I
loss or the inability to use or understand spoken or
language; it may exist without intellectual impairment 1. Sensory (receptive aphasia) – inability to comprehend or understand oral or written communication 2. Motor (broca’s) aphasia can’t speak, write although can comprehend 3. Global aphasia – an almost total language loss manifested in minimal response in every phase of language 4. Auditory aphasia – difficulty of understanding spoken word 5. Nominal aphasia – inability to attach meaning to words read inability to read, word blindness inability to express oneself in writing 1. Absolute – complete inability to write 2. Acoustic – inability to write words head 3. Cerebral – inability to express thoughts in writing 4. Motor- inability to write due to muscle coordination 5. Optic – inability to copy words INTRACRANIAL HEMORRHAGE bleeding beneath the cranium and outside the dura, -
hemorrhage between the dura and arachnoid;
develop slowly; personality changes maybe the first noticeable sign Subarachnoid Hemorrhage hemorrhage between the arachnoid and pia mater into CSF NEUROLOGIC SIGNS increasing or widening pulse pressure Decreasing PR Increasing headache Pappil edema Decreased mental awareness Decreased in RR B. Other signs and symptoms which may or may not develop: 1. Vomiting – may or not be projectile 2. Motor deficits – weakness or paralysis of any part of the body 3. Sensory Disturbances of any part of the body 4. Awkwardness – may mean weakness; difficulty or coordination 5. Speech disturbances 6. Convulsion 7. incontinence/retention C. Localizing Symptoms 1. Frontal Lobe – aphasia A. Cardinal symptoms:
Confusion Changes in personality Jacksonian convulsion- convulsion begins in one part of the body and 2. 3. rubber 4. 5.
spread in orderly manner to all of the body parts. Parietal Lobe – convulsion, sensory disturbance, asteriognosis Temporal Lobe – defects in visual field, taste or hearing, smell of burning
Occipital Lobe – visual disturbance Cerebellum Ataxia – muscle coordination especially manifested when voluntary muscular movements are attempted. Tremors, nystagmus, hypotonia 6. Basal Ganglia Athetosis, chorea, hemiballismus, tremor
Pathopysiology Cause: excessive alcohol consumption, reduced protein intake, exposure to certain chemicals or infectious schistosomiasis ↓ Episodes of necrosis involving the liver cells ↓ Destroyed liver cells are replaced by scar tissue, the amount of which in time may exceed that of the functioning liver tissue ↓ Early in the disease, the liver is apt to be large and its cells loaded with fat ↓ Later as replacing scar tissue contracts, it becomes small ↓ Also, its surface often becomes rough, bec the scar within it is disposed in coarse bundles, which contract and pull in the capsule at certain points and cause the island of residual normal tissue and of new regenerating liver tissue to project in the little lumps ↓ Liver Enlargement → Activity Intolerance r/t fatigue ↓ Portal Obstruction and Ascites → Ineffective Breathing Pattern r/t ↓ intra- abdominal fluid collection (ascites)
Infection and peritonitis compromised ↓ Gastrointestinal varices altered clotting ↓ Edema compromised ↓ Vit deficiency and anemia ↓ liver Mental deterioration inability of the liver
Body Image Disturbed r/t personal vulnerability → Impaired Skin Integrity r/t immunologic status → Risk for Injury and bleeding r/t Mechanism → Fluid Volume Excess r/t →
regulatory mechanism Nutrition Imbalanced: less than body requirements r/t oral intolerance and Cirrhosis → Risk for acute confusion r/t to detoxify certain enzymes or drugs
Prioritization of Problems: 1. Nutrition Imbalanced: less than body requirements r/t oral intolerance and liver cirrhosis - overt 2. Ineffective Breathing Pattern r/t intra- abdominal fluid collection (ascites) overt 3. Fluid Volume Excess r/t compromised regulatory mechanism - overt 4. Impaired Skin Integrity r/t compromised immunologic status - overt 5. Activity Intolerance r/t fatigue - overt 6. Body Image Disturbed r/t personal vulnerability - overt 7. Risk for Injury and bleeding r/t altered clotting mechanism -covert 8. Risk for acute confusion r/t inability of the liver to detoxify certain enzymes or drugs – covert
Assessment
Pathophysiolog y
Objectives
S: “Nahihirapan akong huminga”
Cause: excessive alcohol consumption, reduced protein intake, exposure to certain chemicals and infectious schistosomiais
STO: After 8 hours of health care interventions pt will be free of dyspnea, cyanosis, w/ ABG’s and vital capacity w/in acceptable range LTO: After 2 weeks of health care intervention pt will establish a normal effective respiratory pattern
O: v/s Temp: 36.7°C BP: 110/60 mmHg PR: 94/min RR: 18/min Conscious: dyspheric Prefers to be in bed Prefers to sleep Assisted w/ ADL by SO Easily fatigued: pallor Appears weak and restless On O2 at 12\LPM/NC Irritable thus changes position once in a while (+) coughing, nonproductive Enlarged
Necrosis of liver cells Destroyed liver cells are replaced by scar tissue Scar tissue exceeds that of functioning liver tissue
Portal obstruction and ascites Ineffective Breathing Pattern
Intervention DX: Monitor respiratory rate, depth and effort
Auscultate breath sounds, noting crackles, wheezes, rhonchi Investigate changes in level of consciousness
Monitor temp. note presence of chills, increased coughing, changes in color/character of sputum Monitor serial ABG’s pulse oximetry, vital capacity measurements, chest x-rays Tx: keep head of bed elevated.
Rationale
Evaluation
Rapid shallow respirations/dyspne smay be present bec. Of hypoxia and or fluid accumulation in abdomen Indicates developing complications, increasing risk of infection
STO: fully met pt is no longer dyspheric and O2 is no longer needed
Changes in mentation may reflect hypoxemia and respiratory failure w/c often accompany hepatic coma.
LTO: fully met if pt will establish a normal or effective respiratory pattern
Indicative of onset infection ex. Pneumonia
Reveals changes in respiratory status developing pulmonary complications
Factors: Pt is very cooperative and willing to participate in any therapy
abdomen (ascites)
Position on sides
A: Ineffective Breathing Pattern r/t Ascites
Provide supplemental o2 as indicated
Conserve pt’s strength by providing rest periods and assisting with activities Change position in every 2 hours Assist with paracentesis or thoracentesis as indicated
Ed Encourage frequent repositioning and deep breathing exercises/cough ing as appropriate Demonstrate
Facilitates breathing by reducing pressure on the diaphragm and minimizes risk of aspiration of secretions Maybe necessary to treat/prevent hypoxia. If respiration/oxygena tion inadequate/ mechanical ventilation maybe required Reduces metabolic and oxygen requirements
Promotes expansion and oxygenation of all areas of the lungs Paracentesis and thoracentesis are performed to remove fluid from the abdominal and thoracic cavities respectively.
with respiratory adjuncts
Aids in lung expansion and mobilizing secretion
Reduces incidence of atelectasis, enhance mobilization of secretions Assessment
Pathophysiolog y
Objectives
S: “wala akong ganang kumain”
Cause: excessive alcohol consumption, reduced protein intake, exposure to certain chemicals and infectious schistosomiais
STO: After 8 hours of health care intervention pt will be able to demonstrate progressive weight gain toward goal with pt appropriate normalization of laboratory values LTO: After 1 month of health care interventions pt will attain desirable weight with optimal
O: v/s Temp: 36.7°C BP: 110/60 mmHg PR: 94/min RR: 18/min Conscious Always in bed and asleep Appears weak and restless Globular or enlarged abdomen
Necrosis of liver cells Destroyed liver cells are replaced by scar tissue Scar tissue
Intervention DX: Measure dietary intake by calorie count Weigh as indicated, compare changes in fluid status, recent weight history, skin fold measurement.
Rationale
Evaluation
Provide information about intake needs or deficiencies It maybe difficult to use weight as indicator of nutritional status in view of edema and ascites. Skin fold measurement are useful in assessing changes in muscle mass and
STO: not met Pt was not able to demonstrate progressive weight gain Factors: Pt doesn’t like to eat because he claims that he is already full Recommendation : Pt needs encouragement NGT insertion
Prominent abdominal veins Tenderness on all quadrants Dull abdomen upon percussion Anorexia: food intolerance Slender body built Increased bowel sounds Oral intolerance (-) nausea and vomiting (-) fever (-) diarrhea
exceeds that of functioning liver tissue Vit deficiency and anemia Nutrient imbalanced: less than body requirement
maintenance of health
Tx: Provide diet high in carbohydrates with protein intake consistent with liver function Elevate head of bed during meals.
Offer smaller, more frequent meals Provide salt substitutes, if allowed, avoid those containing ammonia
Restrict intake of caffeine, gas producing or spicy and excessively hot or cold foods.
subcutaneous fat reserves. Provide calories for energy, sparing protein for healing
Reduces discomfort from abdominal distention and decreases sense of fullness produced by pressure of abdominal contents and ascites in the stomach. Decreases feeling of fullness, bloating Salt substitutes enhance the flavor of foods and aid in increasing appetite ammonia potentiates risk for encephalopathy. Aids in reducing gastric irtrtation/diarrhe
LTO: fully met if pt will attain desirable body weight with optimal maintenance of health Not met: If pt will not attain desirable body weight with optimal maintenance of health
Promote undisturbed rest periods especially before meals Provide oral hygiene before meals aesthetically pleasing setting at mealtime Ed: Suggest soft foods, avoiding roughage if indicated. Recommend cessation of smoking. Encourage pt to eat meals and supplementary feedings
a and abdominal discomfort that may impair oral intake and digestion. Conserving energy reduces metabolic demands on the liver and promotes cellular regeneration. Promotes appetite and sense of wellbeing.
Hemorrhage form esophageal varices may occur in advanced cirrhosis. Reduces excessive gastric stimulation and risk of irritation or bleeding. Encouragement is essential fo the pt w/ anorexia and gastrointestinal discomfort.
NEUROLOGIC INFECTIONS BACTERIAL MENINGITIS - Is an inflammation of the arachnoid, pia, and intervening CSF. The infection spreads throughout the subarachnoid space about the brain and spinal cord and usually involves the ventricles. FACTORS PREDISPOSING TO BACTERIAL MENINGITIS head trauma systemic infection post surgical infection meningeal infection other systemic illness When pathogenic organisms enter the subarachnoid space >inflammatory reaction (CFS clouding, exudates formation, changes in subarachnoid arteries (e.g., engorgement with blood, rapture, thrombosis), and congestion of adjacent tissues. The pia arachnoid becomes thickened and adhesions form, especially in the basal cisterns. Little change occurs in brain structures in the early stages. Almost any bacteria can enter the body causing meningitis o The most common are: Meningoccocus (Neisseria meningitides) Pneumococcus (Streptoccous pneumonia) Haemophilus influence These organisms are often present in nasopharynx. It is not known how they enter the blood stream and the subarachnoid space. Clinical manifestations Headache Prostration Chills Fever N/V
Backpain Stiff neck Generalized seizures Later stage, confused, stuporous, or semicomatose, petechial, or hemorrhagic rash may develop The patient may be irritable at first, but as the infection progresses the sensorium becomes clouded and coma may develop o Signs of meningeal irritation: Nuchal rigidity (rigidity of the neck) Positive finding of Brudzinski’s sign Positive finding of Kernig’s sign MENINGITIS infectious organisms gain access to meninges and subarachnoid spaces (viral, bacterial, yeast) Exudate forms ↓ Meningeal irritation/inflammation ↓ Cortical inflammation ↓ Cerebral edema ↓ Increased I ↓ Vasculitis Increased infection Petechial Hemorrhages Neuritis Hydrocephalos ↓ ↓ ↓ ↓ ↓ Cortical Brain abscess Septic Emboli Cranial nerve Increased Necrosis Septicemias involvement I ↓ ↓ ↓ Adrenal DIC Seizures Compression of Hemorrhage brain structures Hemorrhage
Hypoxia Inadequate perfusion Shock ↓ DEATH
HEADACHES
Is a symptom of an underlying disorder rather than a disease itself. The cause must be identified so that appropriate treatment can be given. Clients often-self treat headaches with OTC medication without prescription. Most headaches do not indicate serious disease however; the nurse should encourage clients with persistent or recurrent headaches to seek neurologic assessment. Serious disorders that typically produce headache include intracranial tumors and infection, bacterial or viral meningitis, head injuries, cerebral hypoxia, severe HPN, acute or chronic diseases of the eye, nose, ear, throat. COMMON TYPES OF HEADACHES I. Migraine - Are paroxysmal disorders characterized by recurrent throbbing headaches - Episodes begin during puberty or ages 20-40 years - They decrease in frequency and severity with advancing years - Affects 5-10% of the population - Women are more susceptible than men are - Occurs at irregular intervals, frequency varies from several times a week to several times a year PATHOPHYSIOLOGY (vascular theory is currently accepted) - Constriction of intracranial vessels > neurologic symptoms - Intense throbbing headache is due to dilation of extracranial and intranial branches of the external carotid artery Psychological factors influence migraine headache o Perfectionist o Fatigue o Excess sleep o Hunger o Refractive errors o Bright light o Surprises o Mental and emotional excitement o Excessive smoking o High altitudes o Drinking alcoholic beverages Certain foods that seem to precipitate migraine episodes, food containing beta-phenylethylamine o Chocolate o Cheese o Citrus fruits o Coffee o Pork products o Dairy products Familial tendency
Oral contraceptive may exacerbate migraines or induce their onset in women previously free from significant headaches. It can occur during menstruation. I.1. Classic or Typical Migraine o Preceded by an aura or prodromal phase in which the client may feel depressed, irritable, restlss, and perhaps anorexic o May experience transient neurologic disturbances (visual phenomena, e.g., flashes of lights, bright spots, distorted vision, diplopia), vertigo, nausea, diarrhea, abdominal pain, paresthesis (numbness of tingling of lips, face, or extremities); may lasts a few minutes or several hours. o Has a “cresendo” quality. It gradually increases in severity until the pain becomes intense and all-encoming.>mild discomfort, >prostrating, throbbing pain >seclusion and lie in bed in a darkened room. o Pain described as dull and boring, pressing, throbbing, or hammering. o Unilateral and may be localized to the front, back, or side of the head, often the temple and eye areas. o Acute migraine episodes lasts 4-6 hours (accompanied by photophobia, N/V, vertigo, tremor, diarrhea, excessive sweating or chilliness). o General sensitivity of all sensory organs and client withdraws from light and sound. o Arteries of the head may become prominent and the amplitude of their pulsation increase, scalp may be very tender, swelling, redness, and excessive tearing of the eyes, and swelling of the nasal mucosa (sometimes accompanied by epistaxis) may occur. I.2. Atypical or Common Migraine o Begins suddenly with or without prodromal symptoms, may be generalized or unilateral, and may or may not be accompanied by N/V. MANAGEMENT: 1. Treat the two phases of migraine, vasoconstriction and vasodilation, analgesics such as acetaminophen may relieve mild H/A. 2. Severe headaches respond to ergot preparations but only if they are taking 30-60 minutes after headache onset. Ergot must be taken before the vessels become rigid from edema in their walls. - Prescribed orally IV or rectally - Once the migraine becomes intense ergot is of little value, stronger analgesic such as codeine sulfate, diphenhydramine hydrochloride (Benadryl). 3. Apply pressure on the common carotid artery and the affected superficial artery. 4. Lying in a dark, quiet room with ice on the back of the neck during acute episodes. 5. Relaxation techniques, bio, or counseling directed at preventing episodes by helping the client understand tensions and resolve major life conflicts. 6. Follow a restrictive diet, avoid food and beverages that contain tyramine and have vasoactive qualities. II. Cluster headaches (Histamine headaches)
-
-
Sometimes classified as a form of migraine. Most clients experiencing cluster headaches do not have a history of migraine headaches. Excruciating painful, unilateral , and tend to occur in clusters. There is usually no aura. Episodes may occur within a few days, weeks, or occasionally months, followed by a remission with no symptoms for months or years. Then the headaches again recur in clusters. Cluster headache may recur at irregular intervals for many years, often related to times of stress anxiety, or emotional upset. Men are affected five times more often than are women. Episodes usually begin in middle life and are often worsened by alcoholic consumption. The mechanism underlying cluster headache is not well understood but is believed to be in vascular origin. These headaches were formerly believed to be caused by sensitivity to histamine. During episode, the client experiences: Excruciating, throbbing, or steady pain arising high in the nostril and spreading to one side of the forehead, around and behind the eye on the affected side. The nose and affected eye water, and the skin reddens on the affected side Nasal congestion and conjunctival infection are common. Intervention is ineffective because of shortness of episodes.
MANAGEMENT: 1. Lying in a dark, quiet room with ice on the back of the neck during acute episodes. 2. Indomethacin (Indocin) medication of choice 3. Tricyclic antidepressant 4. ive care – clients tend to become depressed over their condition and fearful recurrent episodes. Some feel they cannot survive another episode. III. Tension headaches (muscle Contraction Headaches) - Results from the long-sustained contraction of skeletal muscles around the scalp, face, and neck and upper back. - Muscles become tender → client tenses more (primary source of many headaches associated with excessive emotional tension, anxiety and depression.) - Vasodilation of associated cranial arteries may also contribute to muscle irritability and head pain - Begin in adolescence but occur most often in middle age. They may increase significantly in menopause. Pre-menstrual headaches are of this type. - Pain is steady, non-pulsatile ache (unilateral or bilateral) in any region of the head, but more so in the occipital and upper cervical regions and extends diffusely over the top of the head - Onset is gradual, with N/V (late reaction), could also be accompanied by dizziness, tinnitus or lacrimation - Pain could be precipitated by combing the hair, wearing a hat or exposure to cold - Maybe unrelieved for weeks, months or years.
MANAGEMENT: 1. Eliminate source of stimulation (diseased teeth) 2. Psychotherapy for those with prolonged and recurrent muscle tension headaches of psychological in origin 3. Symptomatic relief: massage affected muscles, apply local heat, rest and various relaxation techniques 4. Responds well to a combination of non-narcotic analgesic with an anxiety relieving drug, occasionally a stronger analgesic is needed (e.g., Codeine sulfate).
CLIENT EDUCATION GUIDE
PREVENTING MIGRAINE HEADACHES Many things can trigger a migraine headache. It is important for the client to find out what triggers the headache and avoid the trigger, if possible; if avoidance of the trigger is not possible, the dose of medication can be adjusted. Adjusting Medications During Menstrual Cycles. Menstruation and ovulation may trigger migraines. If medications are taken for migraines, a larger dose may be required during these times. Adjusting Dietary Triggers. Alcohol increases the size of blood vessels (vasodilation) and may increase headache. Some foods contain betaphenlethylamine and should be considered possible triggers. These items include chocolate, cheese, citrus fruits, coffee, pork products and dairy products. The lack of eating may lower blood sugar and may lead to headache. In this case, small frequent meals may avert headaches. Identifying the Role of Stress. Stress may trigger migraines. If stressors cannot be reduced, then medications may need to be increased. Heat intolerance (such as vacationing in warm climates) may increase headaches. Other factors related to stress that might trigger headaches include fatigue, excess sleep, and bright sunlight causing a glare from water, roads, or car hoods.
HEMOPHILIA • • • • • • •
A disorder characterized by impaired coagulation of blood and a tendency to bleed. Hereditary coagulation disorder. both hemophilia A (Factor VIII deficiency) and Hemophilia B (Factor IX deficiency) are inherited as sex linked recessive disorder and are therefore almost exclusive for males. Hereditary and limited to males. X-linked recessive disease – it means that, it is common to males but is being transmitted by females. All daughters of hemophiliacs become carrier. Transmitted by a female trait carrier Absence deficiency or malfunction of any one of clotting factors
TRANSMISSION OF HEMOPHILIA Genotype of parents Carrier+N male N female+Hemophiliac Carrier+hemophiliac
N
Female Carrier
50% 0%
50% 100%
Hemophili ac 0% 0%
0%
50%
50%
COMMON TYPES OF HEMOPHILIA 1. Hemophilia A (Classic Hemophilia) • 80% hemophiliacs • Factor VIII deficiency (anti hemophilic factor)
Male N Hemophilia c 50% 50% 100% 0% 50%
50%
2. Hemophilia B (Christmas Factor) • Factor IX deficiency (Plasma Thromboplastin component) 3. Hemophila C • Factor XI deficiency (Plasma Thromboplastin antecedent) STAGES 1. Mild: clotting factor level 6 to 30% • Bruise easily, tendency to nose/gum bleeding 2. Moderate:2 to 5 % • More frequent bleeding episodes; excessive bleeding after surgery or trauma 3. Severe: 1% or less • Spontaneous bleeding; severe bleeding • Hemarthrosis
MANIFESTATIONS: • Diagnosed usually in infancy or early childhood • History of excessive bleeding into any part of the body sponataneoulsy following trauma • History of excessive bleeding following circumcision and dental extraction • PTT of Hemophilia A and hemophilia B is prolonged • Platelet count and prothrombin time is normal TREATMENT • Replace deficient coagulation factor when bleeding episodes do not respond to local treatment (ice bags, manual pressure or dressing, immobilization, elevation and topical coagulants such as fibrin foam and thrombin) • Since the deficient factors are contained in the plasma, fresh plasma and blood or fresh frozen plasma Is given. • In major hemorrhage, adequate blood levels were difficult to maintain without overloading person’s circulation with large volumes of blood and plasma. • In classic hemophilia, treatment of choice in acute bleeding is infusion of concentrate of antihemophilic factor (Factor VII) • Concentrates prevent circulatory overload and produce fewer adverse effects • Usually people who are being transfused with Factor VIII concentrates are easy to acquire AIDS because donors are not screened that well MANAGEMENT: I. Blood Factor replacement Therapy FFP: all clotting factors present Cryoprecipitate: factor VIII, fibrinogen
Lyophilized factor VIII concentrates Vit. K dependent complex: Factor VIII, IX, XI, prothrombin II. Desmopessin for Mild Hemophilia A It triggers the release of Factor VIII CLOTTING FACTORS 1. Factor I – Fibrinogen 2. Factor II – Prothrombin 3. Factor III – Thromboplastin 4. Factor IV – Calcium 5. Factor V – Proaccelerin, labile factor, accelerator globulin 6. Factor VI – omitted 7. Factor VII – Proconvertin, stabile factor, serum prothrombin conversion accelerator (SPCA) 8. Factor IX – Plasma thromboplastin component (PTC) 9. Factor X - Stuart power factor 10.Factor XI – Plasma Thromboplastin antecedent (PTA) 11.Factor XII – Hageman Factor (HF) 12.Factor XIII – Fibrin Stabilizing Factor Extrinsic System
Intrinsic System
Factor III
Factor XII
Factor VII
Factor XI Factor IX Factor VIII
Scheme of clotting Mechanism
Platelet lysis
Factor X Factor V Calcium Prothrombin
Thrombin
Plasminogen Activator Urokinase Plasminogen
Plasmin
COMMON BLEEDING AND COAGULATION BLOOD TESTS TEST Bleeding time
Clotting time (CT) Prothrombin Time (PT)
Partial Thromboplastin Time (PTT) Activated Partial Thromboplastin (APTT)
DESCRIPTION -Evaluation of vascular platelet factors – the time it takes for a small stab wound to stop bleeding -time required for solid clot to form (less sensitive test than PTT) -indicates rapidity of blood clotting (indicates adequacy of extrinsic coagulation pathways for factors I, II, V, VII and X) -more sensitive test than PT to evaluate adequacy of intrinsic coagulation pathway (Fibrin formation) -modified PTT; more sensitive; quicker to perform, frequently used to monitor heparin therapy and hemoglobin
NORMAL VALUES 2 to 9 minutes
5 to 10 minutes 11 to 16 seconds
60 to 90 seconds
26 to 42 seconds
HYPERTENSION: • Elevated blood pressure • A sustained blood pressure greater than 90 mmHg or a sustained systolic pressure in excess of 140 mmHg is considered to constitute hypertension. • About 90-95 of hypertension is idiopathic and apparently primary (Essential hypertension) • Of the remaining 5-10%, most is secondary to renal disease or less often, to narrowing of the renal artery, usually by an atheromatous plaque (Renovascular hypertension) • Infrequently, secondary hypertension is the result of disease related to the adrenal glands. REGULATION OF NORMAL BLOOD PRESSURE: The magnitude of the arterial blood pressure depends on two hemodynamic variables: a. Cardiac output b. Total peripheral resistance CARDIAC OUTPUT: • Influenced by blood volume, which Is greater dependent on body sodium • Thus, sodium homoestasis is central to blood pressure regulation TOTAL PERIPHERAL RESISTANCE: • Predominantly determined at the level of the arterioles and depends on lumen size, itself dependent on the thickness of the arteriolar wall and the effects of neural and hormonal influences that either constrict or dilate these vessels.
• Normal vascular tone depends on the competition between: a) Vasoconstricting influences Angiotensin II Catecholamines Thromboxane Leukotrienes Endothelin b) Vasodilators: Kinins Prostaglandins Nitric oxide •
•
• • •
Certain metabolic products…. a. Lactic acid b. Hydrogen ions c. Adenosine And hypoxia…can also function as local vasodilators!
GENETIC FACTORS: It is now thought that essential hypertension results from an interaction of genetic and environmental that affect cardiac output or both. ENVIRONMENTAL FACTORS: Environmental factors are thought to contribute to expression of the genetic determinants of increased pressure. Stress, obesity, physical inactivity, and heavy consumption of salt have all been implicated as exogenous factors in hypertension. In both the major pathways for hypertension – primary renal and primary vascular defects – heavy sodium intake augments hypertension. MECHANISMS: • What then are the primary defect in essential hypertension? • Two overlapping pathways are proposed: a. Renal retention of excess sodium The existence of genetic factors that result in reduced renal sodium excretion – in the presence of normal arterial pressure – as the initiating event. Decreased in sodium excretion leads to an increased in fluid volume and a high cardiac output. In the face of an increasing cardiac output, peripheral vasoconstriction occurs as a result of auto regulation to prevent the over perfusion of tissues that would ensue from an increase cardiac output. Auto regulation leads to an increase in peripheral resistance, however, and along with it an elevation of blood pressure.
At the higher setting of blood pressure, enough additional sodium can be excreted by the kidneys to equal intake and prevent fluid retention. Thus, an altered but steady state of sodium excretion is achieved (resetting of pressure natriuresis) but at the expense of stable increases in blood pressure b. Vasoconstriction and vascular hypertrophy Such increased resistance is caused either by factors that induce functional vasoconstriction or by stimuli that induce structural changes in the vessel wall like a. Remodeling b. Hypertrophy c. Hyperplasia of smooth muscle cells Leading to thickened wall and narrowed lumen or by both effects. Vasoconstrictive influences may consist of: 1. Behavioral or neurogenic factors – as exemplified by the reduction of blood pressure achieved by meditation (therelaxation response 2. Increase released of vasoconstrictor agents (eg. Rennin, catecholamines, endothelin) 3. Increased sensitivity of vascular smooth muscle to constricting agents. Such vasoconstrictive influences, if exerted chronically, or repeatedly may themselves cause structural thickening of the resistance vessels, thus perpetuating increased blood pressure. Certain vasoconstrictors (eg. Angiotensin II) also function as growth factors causing smooth muscle hypertrophy, hyperplasia and matrix deposition. Conversely, there is evidence that structural changes in the vessel wall may occur early in the hypertension, preceding rather than strictly secondary to the vasoconstriction. Such evidence has led to a hypothesis that genetic or environmentally induced defects in intracellular signaling in smooth muscle cells affect cell cycle genes and ion fluxes that modulate both smooth cell growth and increased vascular tone resulting in wall thickening and vasoconstriction respectively. SUMMARY: • Essential hypertension is a complex disorder that almost certainly has more than one cause. • It may be initiated by environmental factors – stress, salt intake, estrogens… Which affect the variables that control blood pressure in the genetically predisposed individual. • In established hypertension, both increased cardiac output and increased peripheral resistance contribute to the increased pressure. VASCULAR PATHOLOGY:
• •
Hypertension accelerates atherogenesis and causes structural changes in the walls of blood vessels that potentiate both aortic dissection and cerebral hemorrhage. Hypertension is associated with two forms of small blood vessel disease. a. Hyaline arteriosclerosis b. Hyperplastic arteriosclerosis Both lesions are related to elevations of blood pressure, but other causes may also be involved.
HYALINE ARTERIOSCLEROSIS: • The vascular lesion consist of homogenous, pink hyaline thickening of the walls of arterioles with loss of underlying structural detail and with narrowing of the lumen. • It is believed that the lesions reflect leakage of plasma components across vascular endothelium and increasing extracellular matrix production by smooth muscle cells. • Presumably, the chronic hemodynamic stress of hypertension or a metabolic stress in diabetes accentuates endothelial injury, thus resulting in leakage and hyaline deposition. • The narrowing of the arterial lumens causes impairment of the blood supply to affected organs particularly well exemplified in the kidneys. • Thus, hyaline arteriosclerosis is a major morphologic characteristic of benign nephroscerosis in which the arteriolar narrowing causes diffuse renal ischemia of the kidneys. HYPERPLASTIC ARTERIOSCLEROSIS: • Related to more acute or severe elevation of blood pressure and is therefore characteristic of but not limited to malignant hypertension (diastolic pressure more than 110 mmHg). • This form of arteriolar disease can be identified with the light microscopy by virtue of its onion skin, concentrated laminated thickening of the walls of arterioles with progressive narrowing of the lumens. Note: • The kidneys play a very important role in blood pressure regulation. • Renal dysfunction is essential for the development and maintenance of both essential and secondary hypertension. • The kidney influences both peripheral resistance and sodium homeostasis, and the rennin-angiotensin system appears central to these influences. • Rennin elaborated by the juxtaglomerular cells of the kidney transforms plasma angiotensin to angiotension I. • angiotension I is converted to angiotension II by angiotension converting enzyme (ACE) • angiotension II alters blood pressure by increasing both peripheral resistance and blood volume. • Increasing peripheral resistance is achieved largely by its ability to cause vasoconstriction through direct action on vascular smooth muscle.
• •
• • •
Blood volume is increased by stimulation of aldosterone secretion --- which increases distal tubular reabsorption of sodium and thus, of water. The kidney produces a variety of vasodepressor or antihypertensive substances that presumably counterbalance the vasopressor effects of angiotensin. These include: a. Prostaglandins b. Platelet activating factor c. Urinary kalikrein – kinin system d. Nitric oxide When blood volume is reduced; the GPR falls, this, in turn leads to increased reabsorption of sodium by the proximal tubules in an attempt to conserve sodium and expand blood volume. GFR – independent natriueretic factors, including atrial natriuretic factor (ANF), a peptide secreted by heart atria in response to volume expansion, inhibit sodium reabsorption in distal tubules and cause vasodilation. Abnormalities in these renal mechanisms are implicated in the pathogenesis of secondary hypertension in a variety of renal diseases, but they also play important roles in essential hypertension.
PATHOGENESIS OF ESSENTIAL HYPERTENSION: • Arterial Hypertension occurs when changes develop that after the relationship between blood volume and total peripheral resistance. • In renovascular hypertension, renal artery stenosis causes decreased glomerular flow and pressure in the afferent arteriole of the glomerulos and induces rennin secretion by the juxtaglomerular cells. • This initiates angiotension II induced vasoconstriction --- increased peripheral resistance; through the aldosterone mechanism, --- increased sodium reabsorption and increased blood volume. • In Pheochromocytoma, a tumor of the adrenal medulla, catecholamines produced by tumor cells cause episodic vasoconstriction and thus induce hypertension.
PARKINSON’S DISEASE Brain disorder causing progressive deterioration, with muscle rigidity, akinesia, and voluntary tremors Usual cause of death: aspiration pneumonia One of the most common crippling diseases in the United States
Affects more men than women Occurs in middle age or later Pathophysiology: • Dopaminergic neurons degenerate, causing loss of available dopamine • Dopamine deficiency prevents affected brain cells from performing their normal inhibitory function • Excess excitatory acetylcholine occurs at synapses • Nondopaminergic receptors are also involved • Motor neurons are depressed Causes: • Usually unknown • Exposure to such toxins as manganese dust and carbon monoxide Common Characteristics: Muscle rigidity and tremor Resistance to ive muscle stretching Akinesia and dysarthria and drooling High-pitched, monotonous voice, and loss of posture control Excessive sweating and decreased GI motility Orthostatic hypotension and oily skin and eyes fixed upward Complications: injury from falls; food aspiration; urinary tract infections; skin breakdown Assessment: Insidrous (unilateral pill-roll) tremor, which increases during stress or anxiety and decreases with purposeful movement and sleep Dysphagia Fatigue with activities of daily living (ADLs) Muscle cramps of legs, neck, and trunk Increased perspiration and insomnia, mood changes Treatment: • Small, frequent meals and high-bulk food • Physical therapy and assistive devices to aid ambulation • Medication: Dopamine replacement drugs, anticholinergics, antiviral agents, enzyme-inhibiting agents and tricyclic antidepressants • Surgery used when drug therapy fails • Destruction of ventrolateral nucleus of thalamus New research on the pathogensis of Parkinson’s disease focuses on damage to the substantia nigra from oxidative stress. Oxidative stress is believed to: Alter the brain’s iron content Impair mitochondrial function Alter antioxidant and protective systems Reduce glutathione
Damage lipids, proteins, and deoxyribonucleic acid
Nursing Diagnoses: • Interrupted family processes • Imbalanced nutrition: less than body requirements • Bathing or hygiene self-care deficit • Disturbed body image • Chronic low self-esteem • Constipation • Dressing or grooming self-care deficit • Feeding self-care deficit • Impaired physical mobility, social interaction, verbal communication • Ineffective coping and risk for injury The patient will: Perform ADLs and develop alternative means of communicating Avoid injury and maintain adequate calorie intake Express positive feelings about himself Develop adequate coping behaviors and seek resources Nursing Interventions: • Take measures to prevent aspiration • Protect the patient from injury • Stress the importance of rest periods between activities • Ensure adequate nutrition • Provide frequent warm baths and massage • Encourage the patient to enroll in a physical therapy program • Provide emotional and psychological • Encourage the patient to be independent Monitor: Vital signs, intake and output Drug therapy and adverse reactions to medications Postoperatively: signs of hemorrhage and increased intracranial pressure
MYASTHENIA GRAVIS Abnormal fatigability of striated (skeletal) muscles Sporadic but progressive weakness
Muscle weakness exacerbations by exercise and repetitive movement Muscle weakness improved by anticholinesterase drugs Initial symptoms related to cranial nerves With respiratory system involvement, may be life-threatening Spontaneous remissions in about 25% of patients Occurs at any age Three times more common in women than men Highest in women ages 18 to 25, in men ages, 50 to 60 Transient myasthenia in about 20%of infants born to myasthenic mothers
Pathophysiology: • Blood cells and thymus gland produce antibosies that block, destroy, or weaken neuroreceptors (which transmit nerve impulses) • The result is failure in transmission of nerve impulses at the neuromuscular junction Causes: • Autoimmune disorder associated with the thymus gland • Accompanies other immune and thyroid disorders Common Characteristics: Weak eye closure, ptosis and Diplopia Skeletal muscle weakness; paralysis Complications in respiratory distress, pneumonia, aspiration Assessment: Varying assessment findings Progressive muscle weakness Extreme weakness and fatigue (cardiac symptoms) Ptosis and diplopia (the most common sign and symptom) Difficulty chewing and swallowing Jaw hanging open (especially when tired) and Head bobbing Symptoms milder on awakening worsen as the day progresses Short rest periods that becomes more intense during menses, after emotional stress, after prolonged exposure to sunlight or cold, and with infections
Physical Findings: Sleepy, masklike expression
Drooping jaw Ptosis Decreased breath sounds and tidal volume Respiratory distress and myathenic crisis
Treatment: Plasmapheresis Emergency airway and ventilation management Diet as tolerated Activity as tolerated; exercise may exacerbate symptoms Medication: Anticholinesterase drugs, cortiscosteroids, I.V, immune globulin Surgery: Thymectomy
• •
MULTIPLE SCLEROSIS Progressive demyellination of white matter of brain and spinal cord Characterized by exacerbations and remissions
• • • • •
May progress rapidly, causing death within months Prognosis varies (70% lead active lives with prolonged remissions Highest in women, among people in northern urban areas, in higher socioeconomic groups Family history increases with living in a cold, damp climate Major cause of chronic disability in young adults ages 20 to 40
Pathophysiology: • Sporadic patches of demyelination occur in the central nervous system (CNS), resulting in widespread and varied neurologic dysfunction Causes: • Exact cause unknown • Slowly acting viral infection • An autoimmune response of the nervous system • Allergic response • Events that precede the onset: Emotional distress Overwork Fatigue Pregnancy Acute respiratory tract infections • Generic factors possibly also involved Risk Factors: • Trauma, Anoxia, and toxins • Nutritional deficiencies • Vascular lesions • Anorexia nervosa Common Characteristics: • Dependent on the extent and site of myelin destruction • Sensory impairment • Muscle dysfunction • Bladder and bowel disturbances • Speech problems and fatigue • Complications in injuries from falls, urinary tract infections, constipation, contractures, pressure ulcers and pneumonia •
Multiple Sclerosis (MS)described as:
Elapsing remitting – clear elapses with full recovery lasting disability. Between attacks, the disease doesn’t worsen Primary progressive – steady progression or worsening of the disease from the onset with minor recovery or plateaus Secondary progressive begins as a pattern of clear-cut relapses and recovery but becomes steadily progressive and worsens between acute attacks Progressive relapsing – steadily progressive from the onset but also has clear, acute attacks. Differential diagnosis must rule out spinal cord, multiple small strokes, syphilis or another infection, thyroid disease and chronic fatigue syndrome
Assessment: • Symptoms related to extent and site of myelin destruction, extent of remyelination and adequacy of subsequent restored synaptic transmission • Visual problems and sensory impairment (the 1st signs) • Blurred vision or diplopia • Urinary problems • Emotional lability • Dysphagia • Bowel disturbances (involuntary evacuation or constipation) • Fatigue (typically the most disabling symptom) • Poor articulation • Muscle weakness of the involved area • Spasticity; hyperreflexia • Intention tremor and gait ataxia • Paralysis, ranging from monoplegia to quadriplegia • Nystagmus scotoma • Optic neuritis and Ophthalmoplegia Treatment: General for acute exacerbations, for the disease process and for related signs and symptoms High fluid and fiber intake in case of constipation Frequent rest periods Medications: I.V. steroids followed by oral steroids, immunosuppresants, antimetabolics, alkylating drugs, biological response modifiers Nursing Diagnoses: • Activity intolerance • Interrupted family processes
• • • • • • • • • • • •
Imbalanced nutrition: less than body requirements Ineffective role performances Disturbed thought processes Impaired urinary elimination Chronic low self-esteem Constipation Fatigue Impaired physical mobility Compromised family coping Ineffective coping Deficient knowledge chronic pain Risk for infection and injury The patient will: Perform activities of daily living Remain free from infection Maintain t mobility And range of motion Express feelings of increased energy and decreased fatigue Develop regular bowel and bladder habit Use systems and coping mechanism
Nursing Intervention: • Provide emotional and psychological • Assist with physical therapy program • Provide adequate rest periods • Promote emotional stability • Keep the bedpan or urinal readily available because the need to void is immediate • Provide bowel and bladder training if indicated • ister medications • Monitor: o Response to medications o Adverse drug reactions o Sensory drug reactions o Muscle dysfunction o Energy level o Signs and symptoms of infection o Speech o Elimination patterns vision changes o Laboratory results
AMYOTROPHIC LATERAL SCLEROSI Most common motor neuron disease of muscular atrophy Chronic, progressive and deliberating disease that’s invariably fatal No cure Also known as Lou Gehrig’s disease 3 times more common in men than in women Affects people ages 40 to 70
Pathophysiology: • An excitatory neurotransmitter that accumulates to toxic levels • Motor units that no longer innervate • Progressive degeneration of axons that cause loss of myelin • Progressive degeneration of upper and lower motor neurons • Progressive degeneration of motor nuclei in the cerebral cortex and corticospinal tracts Causes: • Exact cause unknown • 10% of patients with amyotrophic lateral sclerosis (ALS) inherit the disease as an autosomal dominant trait • Virus that creates metabolic disturbances in motor neurons • Immune complexes such as those formed in autoimmune disorders Precipitating factor that cause acute deterioration: • Severe stress, such as myocardial infraction • Traumatic injury • Viral infections • Physical exhaustion Common Characteristics: • Muscle weakness • Atrophy • Fasciculations • Respiratory tract infections • Complications of physical immobility Assessment: Mental function intact
Family history of ALS Asymmetrical weakness 1st noticed in one limb Easy fatigue and easy cramping in the affected muscles Physical Findings: Location of affected motor neurons Severity of the disease Fasciculations in the affected muscles Progressive weakness in muscles of the arms, legs and trunk Brisk and overactive stretch reflexes Difficulty talking, chewing, swallowing and breathing Shortness of breath and occasional drooling Treatment: Rehabilitation May need tube feedings No restrictions : as tolerated Medication: muscle relaxants, dantrolene, Baclofen I.V. or intrathecal istration of thyrotropin-releasing hormone Nursing Diagnoses: Imbaanced nutrition: less than body requirements Anticipatory grieving Anxiety Bathing or hygiene self-care deficit Dressing or grooming self-care deficit Feeding self-care deficit Hopelessness Impaired physical mobility Impaired airway clearance Ineffective breathing pattern Ineffective coping Compromised family coping Deficient knowledge (ALS) Risk for impaired skin integrity Risk for infection The patient will: • Maintain a patent airway and adequate ventilation • Maintain t mobility and range of motion (ROM) • Maintain daily calorie requirements
• •
Seek systems and exhibit adequate coping behaviors Remain free from infections
Nursing Interventions: Provide emotional and psychological Teach about active exercises and ROM exercises Promote independence Teach about meticulous skin care Turn and reposition the patient frequently ister ordered medication Teach how to perform deep-breathing and coughing exercises Provide airway and respiratory management Promote nutrition Teach about swallowing regimens and aspirations precautions Monitor: o Muscle weakness o Respiratory status o Speech o Swallowing ability o Skin integrity o Nutritional status o Response to treatment o Complications o Signs and symptoms of infection •
Modifying the home for a Patient with ALS Guidelines: • Explain basic safety precautions, such as keeping stairs and pathways free from clutter, using nonskid mats in the bathroom and in place of loose throw rugs; keeping stairs well lit; installing handrails in stairwells and the shower, tub and toilet areas and removing electrical and telephone cords from traffic areas. • Discuss the need for rearranging the furniture moving items in or out of patient’s care area, and obtaining such equipment as a hospital bed, a commode, or oxygen equipment. • Recommend devices to ease the patient’s and caregiver’s work such as extra pillows or wedge pillows to help the patient sit up, a draw sheet to help him move up in bed, a lap tray for eating, or a bell for calling the caregiver. • Help the patient adjust to changes in the environment. Encourage independence.
•
Advise the patient to keep suction due to handy to reduce the fear of choking due to secretion accumulation and dysphagia. Teach him to suction himself.
GUILLAIN-BARRE SYNDROME A form of polyneuritis Acute, rapidly progressive, and potentiaaly fatal Three • • •
Phases: Acute – lasting from 1st symptoms, ending in 1 to 3 weeks Plateau – lasting several days to 2 weeks Recovery – coincides with remyelination and axonal process regrowth; extends over 4 to 3 years; recovery possibly not complete
Pathophysiology: Segmented demyclination of peripheral nerves occurs, preventing normal transmission of electrical impulses Sensorimotor nerve roots are affected; autonomic nerve transmission may also be affected Causes: Unknown Virus can cause cell-mediated immunologic attack on peripheral nerves Risk Factors: Surgery Rabies or swine influenza vaccination Viral illness Hodgkin’s or some other malignant disease Lupus erythematosus Common Characteristics: Symmetrical muscle weakness initially in lower extremities and progressing to upper extremities Parethesia Diplegia Dyshagia Hypotonia Areflexia
Complications: Thrombophlebitis Pressure ulcers, contractures and muscle wasting Aspiration and respiratory and cardiac compromise
Assessment: Minor febrile illness 1 to 4 weeks before symptoms Tingling and numbness (paresthesia) in the legs Progression of symptoms to arms, trunk and finally, the face Stiffness and pain in the calves Physical Findings: Muscle weakness (major neurologic sign) Sensory loss, usually in the legs (spreads to arms) Difficulty in taking, chewing and swallowing Paralysis of the ocular, facial and oropharyngeal muscles Loss of position sense Diminishes or absent deep tendon reflexes Diagnostic Procedures: • Cerebrospinal fluid (CSF) analysis may slow a normal white blood cell count, an elevated protein count and in severe disease, increased CSF pressure. Others: • Electromyography may demonstrate repeated firing of the same motor unit instead of widespread sectional stimulation • Nerve conduction studies show marked slowing of nerve conduction velocities Treatment: Primarily ive Possible endocrinal intubation or tracheotomy Volume replacement Plasmapheresis Possible tube feeding with endotracheal intubation Adequate calorie intake Exercise program to prevent contractures I.V. beta-adrenergic blockers and parasympatholytics I.V. immune globulin and possible tracheostomy
Possible gastrotomy or jejunotomy feeding tube insertion Nursing Diagnoses: • Imbalanced nutrition: less than body requirements • Impaired urinary elimination • Anxiety and fear • Impaired gas exchange and impaired physical mobility • Impaired verbal communication and ineffective breathing pattern The patient will: Maintain a patent airway and adequate ventilation Develop alternate means of expressing self Maintain required calorie intake daily Establish routine urinary elimination patterns Maintain t mobility and range of motion (ROM) Nursing Interventions: Establish a means of communication before intubation is required Turn and reposition the patient Encourage coughing and deep breathing Begin respiratory at the first sign of dyspnea Provide meticulous skin care ister ive ROM exercises In case of facial paralysis, provide eye and mouth care Prevent constipation Provide emotional ister medications, as ordered Monitor: o Vital signs o Breath sounds o Arterial blood gas measurements o Level of consciousness o Continual respiratory function o Pulse oximetry o Signs of thrombophlebitis o Signs of urine retention o Response to medications